
February 15, 2026
What Is Sculptra Treatment A Guide to Rebuilding Your Natural Collagen
What is Sculptra treatment? Explore how this unique collagen stimulator works to gradually restore facial volume for natural, long-lasting rejuvenation.
Sep 24, 2025

A successful recovery starts long before you ever get to the operating room. When it comes to pain management after surgery, the work you do ahead of time—talking with your doctors and getting your home ready—can make all the difference in how you feel afterward. It's about taking control and easing your own anxiety.

Think of the time before your operation as your opportunity to lay the groundwork for a much smoother healing process. By being an active participant, you're not just a patient; you're a partner in your own care. This helps your medical team truly understand what you need and expect.
This patient-centered approach is more important than ever. With an aging population and more surgeries being performed, the focus on effective pain control has sharpened. In fact, the global market for postoperative pain management is projected to hit an incredible US$ 65.22 billion by 2032. This isn't just a statistic; it shows a real shift in medicine toward making patients more comfortable after their procedures. You can read more about this trend in this market research on postoperative pain management.
Your surgeon and anesthesiologist are your go-to experts for managing pain. I always tell my patients not to be shy about this. Schedule a dedicated time to talk through the pain management plan, and come with your questions ready.
Here are a few things I’d suggest asking:
The whole point of this conversation is to walk away feeling informed and confident, not more worried. Having a clear plan strips away the fear of the unknown, which can honestly make pain feel worse than it is.
When you get home, the last thing you want to do is struggle. Your space should be set up for rest and healing, not creating extra work. Your mobility might be limited, so a little prep work goes a very long way.
Create a "recovery nest" for yourself—a comfy spot on the couch or in a recliner where you'll spend most of your time. Keep everything you could possibly need within arm's reach: your phone and charger, the TV remote, water, snacks, and your medications.
Stock your kitchen with simple meals and snacks that don't require much effort. And most importantly, line up some help. Ask a friend or family member if they can be on call for those first few days to help with errands, meals, or looking after kids or pets. For an even deeper dive, our guide on how to prepare for surgery has a ton of practical tips to help you get everything in order.
Heading home with a new set of prescriptions can be a little overwhelming. It’s not just about taking a pill when you hurt; it's about understanding what you're taking, why you're taking it, and when to take it. Getting this right is one of the most powerful things you can do for your own recovery.
The goal is to stay ahead of the pain, not chase it.
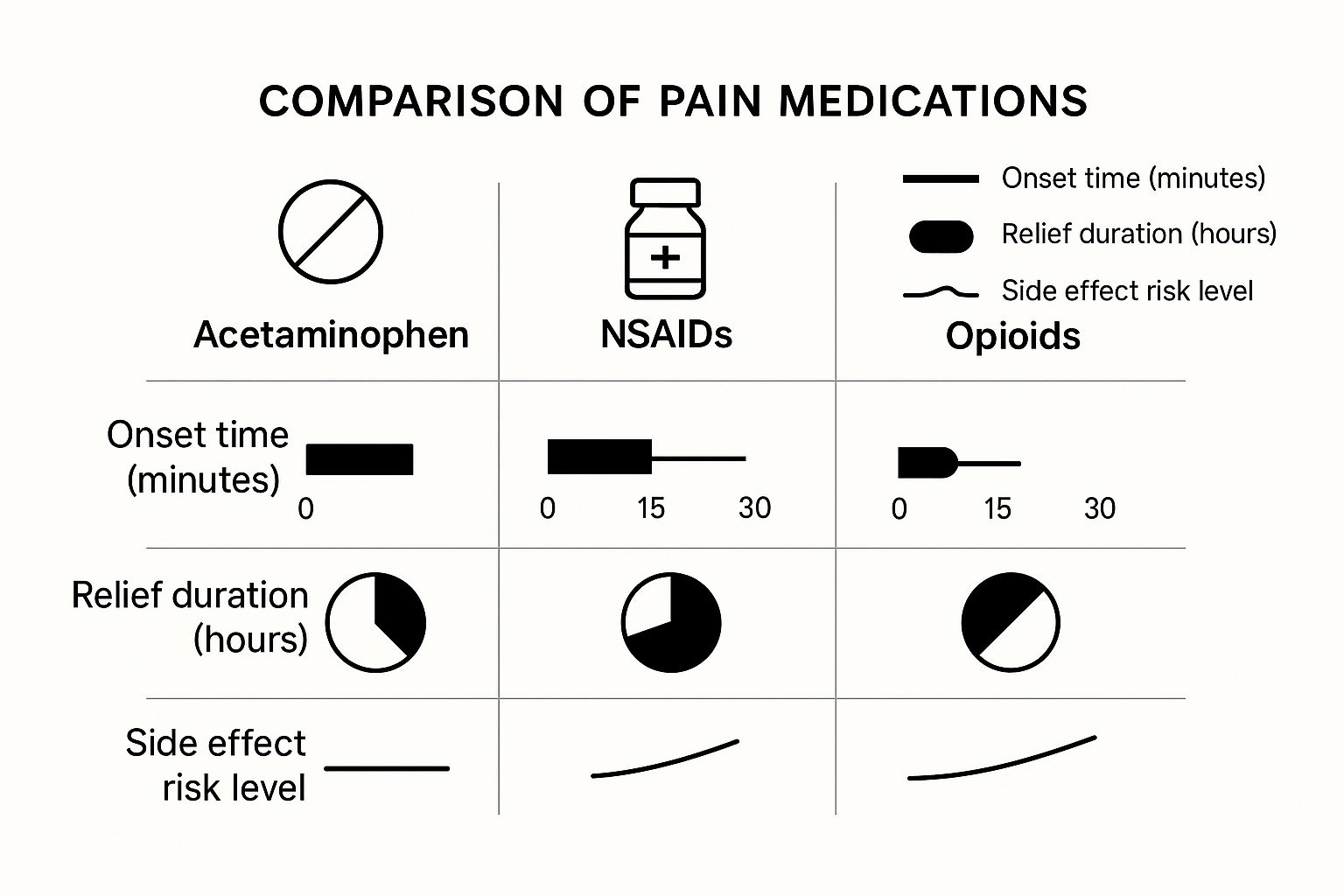
These days, surgeons and pain specialists rely on a strategy called multimodal analgesia. Think of it as a team effort. Instead of using a single, high-dose medication (which can come with more side effects), your doctor combines lower doses of different types of medications. Each one tackles pain from a slightly different angle, giving you better relief with fewer issues.
Your discharge papers will likely list a few different medications. Each has a specific job, and they’re designed to work together to keep you comfortable.
This collaborative approach is changing how we manage recovery. In fact, the market for effective post-operative pain treatments is projected to hit USD 70.6 billion by 2035. With over 33 million opioid prescriptions written in the U.S. in 2020 alone, there's a huge focus on integrating safer, multimodal plans. You can read more about these postoperative pain market projections to see how care is evolving.
So, what might you find in your pharmacy bag? Here's a look at the most common types of medications and what they do.
This table is a starting point. Your personal prescription plan is designed specifically for you, your surgery, and your medical history.
This is the single most important piece of advice I can give you: take your medication on the schedule your doctor gave you.
So many people wait until the pain gets bad before they take their next dose. That’s the biggest mistake you can make. Pain is much easier to keep at bay than it is to reel back in once it’s out of control.
Think of your pain medication as building a wall against the pain. If you take your doses on time, the wall stays strong. If you wait too long, the wall crumbles, and the pain floods in. Rebuilding that wall takes a lot more time and energy.
The first 48 to 72 hours after surgery are often the most challenging. Set alarms on your phone. Use a notepad to log the time you take each medication. This simple step prevents you from accidentally missing a dose or, just as importantly, taking one too soon. It’s your best defense against breakthrough pain.

While the medications your doctor prescribed are a critical part of your recovery, they’re not the only tool in your toolbox. The best pain management after surgery is about layering different strategies. Simple, non-drug techniques can work alongside your medication to make you significantly more comfortable.
Think of it as giving your body a helping hand. These methods support the natural healing process by easing swelling, calming tense muscles, and giving you a sense of control over your own recovery. Often, they can even help you reduce your reliance on pain pills.
Some of the most effective and time-tested tools you have are cold and heat. Knowing when to use each can make a world of difference in your day-to-day comfort.
Cold Therapy: Your Go-To for Swelling
For the first 48-72 hours after your surgery, ice is your best friend. Cold therapy, or cryotherapy, works by constricting blood vessels. This simple action helps reduce the inflammation and swelling that cause that sharp, throbbing pain at the surgical site.
Heat Therapy: For Aches and Stiffness
Once that initial swelling starts to go down (usually after a few days), switching to heat can feel incredibly soothing. Heat does the opposite of cold—it increases blood flow, which helps relax the stiff, achy muscles that often develop around the area you had surgery.
How you position your body in bed or on a chair can have a huge impact on your pain. The goal is simple: use gravity to your advantage to reduce pressure and swelling.
Strategic use of pillows isn't just about feeling cozy—it's a core part of recovery. Elevating the surgical area above the level of your heart is one of the most effective ways to drain fluid, which directly reduces swelling and the throbbing pain that comes with it.
If you’ve had knee surgery, for example, that means propping your entire leg up on a few pillows. After abdominal surgery, a small pillow tucked under your knees can take the strain off your core. Don’t be afraid to experiment to find the position that gives you the most relief.
If you’re interested in complementing your prescribed medications, you can also explore a variety of natural chronic pain relief methods to see if they can improve your comfort.
Managing your pain after surgery is about more than just what's in your pill bottle. It’s about creating the right environment for your body to do what it does best: heal itself. What you eat and how you move have a massive impact on your pain levels and how quickly you get back on your feet.
I know the idea of moving around right after surgery sounds daunting, maybe even a little scary. But staying completely still is one of the worst things you can do. It leads to stiff joints and sore muscles, which just adds to your overall discomfort. More critically, getting up and moving is your number one defense against dangerous complications like blood clots (deep vein thrombosis).
We're not talking about hitting the gym here. The goal is simple: get your blood flowing and prevent your body from getting stiff. Start small. Seriously, a walk from your recliner to the kitchen is a fantastic start.
Here's a practical way to approach it:
Think of gentle movement as lubrication for your body. It keeps everything working smoothly, prevents dangerous clots, and reduces the stiffness that contributes to overall pain, making your recovery much more comfortable.
Right now, your body is a construction zone, working hard to repair tissue. To do that job well, it needs high-quality fuel and the right building materials. Good nutrition can dramatically cut down on inflammation, which is a huge driver of post-op pain.
Focus on whole foods that fight inflammation. You don't have to get complicated, just prioritize a few key things:
When you combine gentle, consistent movement with a nutrient-rich diet, you give your body everything it needs to heal efficiently. Some procedures have their own specific needs, so it can be helpful to look at specialized advice, like these liposuction recovery tips for faster healing that build on these core principles. This two-pronged approach ensures you're tackling recovery from every possible angle.

Some level of discomfort after surgery is completely normal—it’s just part of the healing process. The real challenge is knowing the difference between that expected, manageable pain and a signal that something isn’t right. Learning what to watch for takes the guesswork out of recovery and helps you get help fast if you need it.
Let me be clear: your medical team wants to hear from you if you're concerned. Good pain management after surgery is a team sport, and you're the most important player. The entire medical field is heavily invested in this; North America alone accounts for over 37% of the global market for postoperative pain therapies. You can read more about the postoperative pain therapeutics market on cognitivemarketresearch.com. What this means for you is that protocols are in place to keep you safe, and your doctors are ready to step in at the first sign of trouble.
First things first, never worry that you're "bothering" your care team. I've seen it time and again—it is always better to call and be told everything is fine than to wait and let a minor issue spiral into a major complication.
There are certain symptoms that should have you reaching for the phone right away, day or night. Don't hesitate if you experience any of these:
Trust your gut. You live in your body every day, so if something just feels wrong, that's reason enough to make a call. Being proactive is one of the smartest things you can do for a smooth recovery.
When you do call, being prepared to describe what you're feeling makes a huge difference. "It hurts a lot" is a starting point, but specific details help your doctor or nurse understand the situation much more quickly.
Before you dial, take a moment to think about the pain. Your team will almost certainly ask you to rate it on a 0-10 scale, which gives everyone a shared language to talk about your comfort level.
The 0-10 Pain Scale Explained
Using this scale lets you paint a much clearer picture. For instance, instead of just saying you're in pain, you could say, "This morning after my medication, my pain was a 4. But now, a few hours later, it's a solid 7, and I’m feeling a new, sharp stabbing feeling right next to my incision." That kind of specific, detailed information is incredibly valuable and helps your team give you the best possible advice.
https://www.youtube.com/embed/KdFrlUCRinA
Heading home after surgery can feel a little overwhelming, and it's natural to have a lot of questions pop up as you start to recover. Knowing what’s normal and what isn’t can make a huge difference in your peace of mind. Let's walk through some of the most common concerns I hear from patients about managing pain after their procedure.
This is probably the number one question, and the honest answer is: it completely depends. Every person and every procedure is different.
For a less invasive surgery, you might only need the strong stuff for 2-3 days. After that, many patients find they can comfortably switch over to over-the-counter options like Tylenol or ibuprofen.
On the other hand, a more extensive operation, like a tummy tuck or major joint surgery, could mean you'll need that prescription-level relief for a week or even two. The goal is always the same: use the lowest dose that keeps you comfortable for the shortest time needed. Your surgeon will give you a schedule for tapering off the medication—stick to it rather than stopping suddenly.
Yes, absolutely. In fact, I make a point to warn all my patients about this because it often catches them off guard.
During your surgery, you receive long-acting anesthetics and maybe even a nerve block. These are fantastic for keeping you comfortable initially, but they usually wear off around day two or three. When they do, it's very common to feel a sudden spike in discomfort.
This is precisely why we stress staying ahead of the pain by taking your medication on a strict schedule for those first few days. That said, if the pain becomes severe and you also notice a fever, increased redness, or major swelling, that’s your cue to call your doctor. Those could be signs of a complication.
It's a common misconception that pain should only get better every single day. The reality is that recovery often has peaks and valleys, especially in that first week as your activity level changes and surgical anesthetics fully wear off.
The two biggest culprits here are constipation and nausea. They’re annoying, but you can get ahead of them.
If you're still in the planning stages of your surgery and want to feel fully prepared, we've compiled a list of the top questions patients ask before cosmetic surgery in another guide.
At Cape Cod Plastic Surgery, Dr. Fater and our entire team are here to make sure your journey—from the first conversation to your final follow-up—is as smooth and comfortable as possible. If you have questions about an upcoming procedure, contact us today to schedule your personalized consultation at https://ccplasticsurgery.com.

February 15, 2026
What is Sculptra treatment? Explore how this unique collagen stimulator works to gradually restore facial volume for natural, long-lasting rejuvenation.

February 14, 2026
Learn how to tighten facial skin naturally with proven skincare, exercises, and diet. Our guide offers actionable tips for achieving firmer, more youthful skin.

February 13, 2026
Considering Kybella for under chin fat? Learn how it works, what to expect, costs, and if you're a candidate in our complete guide to jawline contouring.