
February 21, 2026
How to Prevent Keloid Scars After Surgery A Definitive Guide
Discover how to prevent keloid scars after surgery with our definitive guide. Learn expert strategies for risk assessment, surgery, and post-op scar care.
Dec 24, 2025

If you're feeling a bit lost about what to eat before surgery, you're not alone.If you're feeling a bit lost about what to eat before surgery, you're not alone. That old, rigid rule of "nothing after midnight" is thankfully a thing of the past. Today's guidelines are much more focused on keeping you comfortable and well-hydrated, allowing for a light, easily digestible meal up to six hours before your procedure and clear liquids up to two hours before.
Trying to figure out the rules for eating before your operation can feel complicated, but the reason behind them is actually quite simple: your stomach needs to be empty when you go under anesthesia. This is the single most important step to prevent a rare but very serious complication called pulmonary aspiration, which is when stomach contents accidentally get into the lungs.
Think of it like a plumber needing to drain the pipes before starting work—we need a clear field to ensure everything goes smoothly and safely.
But we've also learned that fasting for too long can backfire. Showing up for surgery dehydrated, with low blood sugar, and feeling "hangry" isn't good for anyone. It can make you more anxious, increase the chances of post-op nausea, and can even make it tougher for the nurse to place your IV.
The American Society of Anesthesiologists (ASA) has developed smart, evidence-based guidelines that strike the perfect balance between safety and your comfort. These rules are far more flexible than the old, strict "nothing by mouth after midnight" orders and are designed to be easy to remember. The main goal is simple: get the solid food out of your stomach while keeping your body hydrated.
The easiest way to remember this is the "6-4-2 Rule," a simple guide for the most important cutoffs:
At Cape Cod Plastic Surgery, we follow these updated guidelines to make sure our patients are as safe and comfortable as possible. Sticking to this schedule really helps reduce that pre-surgery thirst and anxiety, making the whole experience much better from the start.
To make things crystal clear, the table below breaks down exactly what you can have and when you need to stop.
Remember, you should always confirm the final instructions with your surgical team, as your specific procedure might have slightly different requirements. Learning more about how to prepare for surgery in general can also give you more context and put any lingering worries to rest.
If you've had surgery before, you probably remember the strict, non-negotiable "nothing by mouth after midnight" rule. For decades, that was the standard of care, leaving patients hungry, dehydrated, and anxious for hours before their procedure. Thankfully, our medical understanding has come a long way, leading to much safer and more comfortable fasting guidelines.
The reason for fasting before surgery has always been about one thing: ensuring your stomach is empty. This prevents a rare but very serious complication called pulmonary aspiration, where stomach contents get into the lungs while you're under anesthesia. Because the body's natural gag reflexes are suppressed during surgery, this is a crucial safety step. You can read more about how different types of anesthesia affect the body in our detailed guide.
But that old, rigid rule was a blunt instrument. Think of your stomach like a sink—it needs to be empty before the plumber (your surgeon) starts work, but that doesn't mean you have to shut off the water 12 hours ahead of time. Modern research has given us a much smarter, more precise approach.
The big shift away from the "NPO after midnight" policy is based on a much better understanding of gastric emptying times, which is just a fancy way of saying how long it takes for food and drink to leave your stomach. Based on this science, the American Society of Anesthesiologists (ASA) developed new, evidence-based guidelines that strike a perfect balance between safety and patient comfort.
Here's the key discovery:
This new knowledge changes everything. Forcing patients to go without clear liquids for many hours isn't just unnecessary; it can actually be counterproductive. Showing up for surgery dehydrated with low blood sugar can create more problems, not fewer.
Modern fasting isn't about being less safe; it's about being more precise. By allowing clear liquids up to two hours before surgery, we can keep patients hydrated and more comfortable, which contributes to better outcomes, including less pre-op anxiety and post-op nausea.
Even with all the clear benefits, getting the entire medical community to adopt these modern guidelines has been a slow process. Many hospitals and surgical centers still cling to the outdated "nothing after midnight" rule, often out of institutional habit or logistical convenience.
In fact, a comprehensive survey of 971 anesthetists revealed a huge gap between official recommendations and what was happening in practice. While 85% of them claimed to follow modern guidelines, a surprising 50.4% admitted they still told patients to stop all fluids at midnight. The main reasons they gave were unpredictable OR schedules and lingering, unfounded fears about the safety of the newer fluid rules.
This disconnect is exactly why it's so important for you, as the patient, to understand the science. It gives you the power to have an informed conversation with your medical team. Knowing that clear liquids are perfectly safe up to two hours before your procedure helps you advocate for your own comfort and well-being.
Ultimately, these updated rules are a major step forward in patient-centered care. They reduce the physical and psychological stress of surgery, ensuring you arrive for your procedure in the best possible condition—hydrated, calm, and ready for a smooth recovery. Always confirm the specific instructions with your surgeon, but rest assured that modern fasting protocols are designed with your safety and comfort as the top priorities.
The final 48 hours before your surgery are your last chance to really load your body up with the nutrients it needs to heal well. Think of it like carb-loading before a marathon—you're stocking up on fuel to get through the main event and recover stronger on the other side. The game plan is simple: eat foods that are both nourishing and incredibly easy to digest. This sets the stage for a much smoother surgical experience.
Your pre-op diet really boils down to three key things: lean protein, smart carbs, and great hydration. This trio works together to support muscle repair, give you sustained energy, and keep your body running like a well-oiled machine. You're giving your system all the good stuff without making it work overtime to break it down.
To keep it simple, just focus on building your meals around these three components. Each one has a specific job to do in getting you ready for the physical stress of surgery and the demands of recovery.
Lean Protein: This is your number one building block for tissue repair and a strong immune system. Getting enough protein helps you hang on to muscle mass, which can take a hit when you’re less active after your procedure. Think chicken breast, fish, tofu, and beans.
Complex Carbohydrates: These guys are all about providing a slow, steady stream of energy to keep your blood sugar from going on a rollercoaster. Unlike sugary snacks that lead to a crash, things like sweet potatoes, brown rice, and oatmeal offer fuel that lasts.
Smart Hydration: This is non-negotiable. Water is always your best friend, but clear broths and electrolyte drinks (the ones without protein or solids) are great, too. When you’re well-hydrated, it’s much easier for the medical team to place your IV, and it helps your body handle the anesthesia more effectively.
What you don't eat is just as critical as what you do. In these last 48 hours, you need to steer clear of anything that's tough to digest, causes inflammation, or leaves a lot of residue behind. Avoiding these foods is the best way to make sure your stomach is truly empty and ready for anesthesia.
You'll want to pass on:
Having a plan for your meals takes all the last-minute stress and guesswork out of the equation. As you get into the final 24 hours, your diet should become even lighter and simpler. For more general strategies on organizing meals, you might find it helpful to look at a comprehensive guide to meal prep planners.
Here’s a look at what a simple, nourishing final day of eating could look like.
Remember, this is just a sample, but it illustrates the core principle: keep it light, simple, and easy on your gut as you approach surgery day.
The most important rule of thumb is to have your final solid meal—even a light one—finished at least six to eight hours before your scheduled surgery time. This gives your body plenty of time to process everything, ensuring you arrive with an empty stomach, which is our absolute top priority for your safety.
As surgery gets closer, the rules about eating and drinking tighten up. It might seem tedious, but these guidelines are absolutely critical for your safety. The goal during this final window is simple: clear your stomach completely while staying properly hydrated.
Think of it like the final prep lap before the main event. We’ll walk through exactly what’s allowed and when, taking all the guesswork out of this crucial period. Following these rules to the letter helps ensure your body is perfectly ready for anesthesia, which minimizes risks and sets you up for a much smoother experience.
This visual guide gives you a clear picture of the pre-surgery eating and drinking schedule, showing how you’ll move from solid foods to only clear liquids.
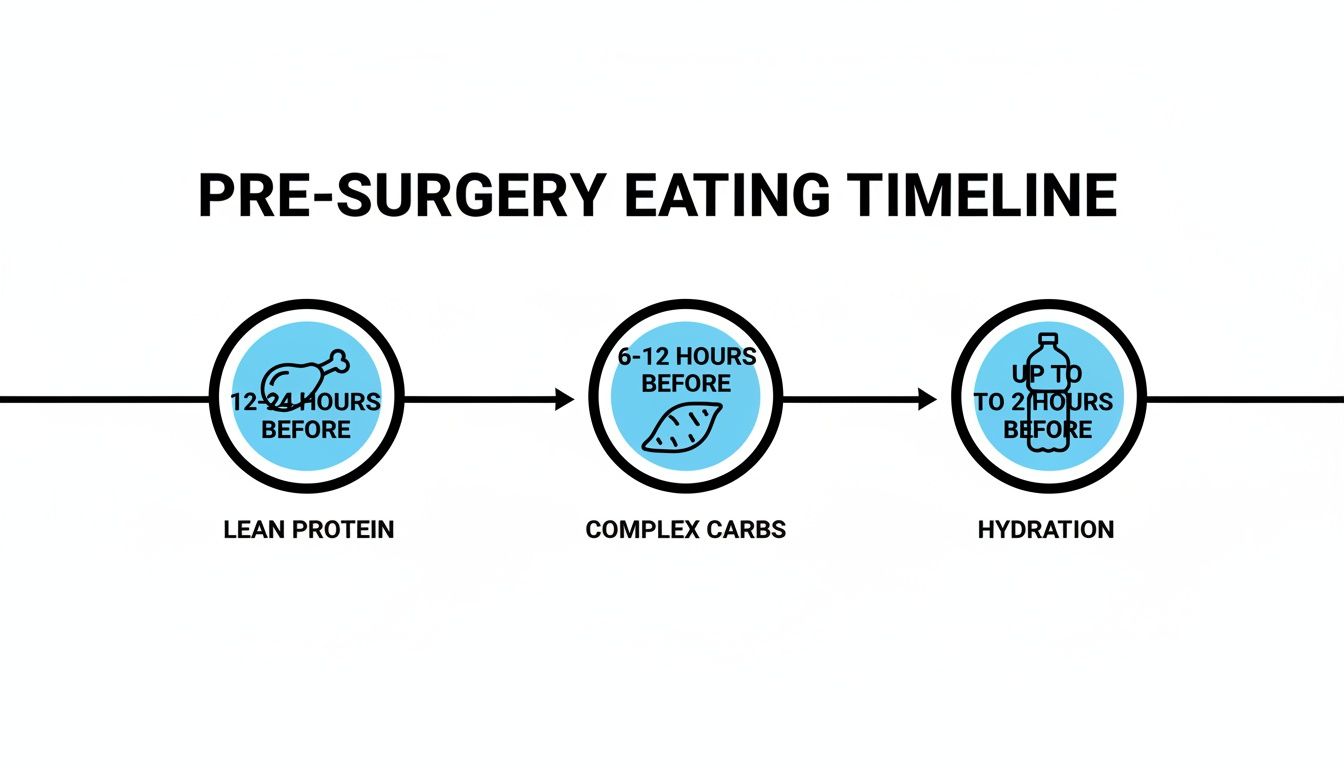
The key is a simple, logical progression. You start by nourishing your body with light, easily digestible foods like lean protein and complex carbs well ahead of time. Then, as your surgery time draws near, you switch exclusively to clear liquids to make sure your system is empty and ready.
Your last chance for any solid food is at least six hours before your scheduled surgery. At this point, you can have what we call a "light meal." In a pre-op context, this term is very specific—this isn't the moment for a big breakfast or anything fatty, greasy, or fibrous.
So, what does a perfect light meal look like? It's small, low-fat, and easy for your stomach to process quickly. Good examples include:
The idea is to give your body a tiny bit of energy without leaving anything behind in your stomach. After this meal, the kitchen is officially closed for solids.
In the window between six and two hours before surgery, we actually want you to drink clear liquids. Staying hydrated is one of the best things you can do for yourself. It helps with thirst and anxiety, and it can even make placing your IV a bit easier for the nursing staff.
But the definition of a "clear liquid" is non-negotiable. It must be something you can see through, with absolutely no solid particles, pulp, or fat. This isn't just a suggestion; it's a critical safety rule.
Here’s a definitive list of what you can drink up until the two-hour mark:
Just as important is knowing what is NOT a clear liquid, even if you can drink it:
If you consume anything from that second list within the six-hour window, we have to treat it as if you've eaten a solid meal. This could mean your surgery gets delayed or even canceled. The two-hour mark is the absolute final cutoff for everything—after that, it's strictly nothing by mouth.
This strict adherence is paramount. We've moved away from outdated, overly cautious fasting rules and embraced more precise, evidence-based timelines. In fact, one recent study showed that properly educating patients and staff on modern fluid rules dramatically reduced over-fasting and lowered complications like dehydration and nausea after surgery. You can read the full research about these fasting improvements to see just how much these modern guidelines improve patient safety.

When you're managing a health condition like diabetes or taking daily medications, getting ready for surgery becomes a bit more complex. It's not just about what you eat; it's about making sure your entire health plan is in perfect sync with your surgical team.
Think of it like this: your body is a finely tuned orchestra. Anesthesia and the stress from an operation can suddenly change the music's tempo. Your medications are key instruments, and some might need to be played differently—or even paused—to keep everything in harmony. This is especially true for our patients with diabetes, as fasting and surgical stress can cause major swings in blood sugar.
Keeping your blood sugar stable isn't just a suggestion—it's absolutely vital for a safe procedure and a smooth recovery. High blood sugar can throw a wrench in your immune system and slow down healing, which nobody wants. This is why we need a crystal-clear picture of your health to make the right calls for your care.
This information is for guidance only and is not a substitute for professional medical advice. The only instructions you should follow are the ones given directly to you by your surgeon and anesthesiologist.
If you have diabetes, the fasting rules require a very specific, personalized game plan. Going hours without food can make your blood sugar plummet (hypoglycemia), while the physical stress of the operation can send it soaring (hyperglycemia). Neither scenario is safe. A good starting point for this conversation with your doctor is understanding your HbA1c levels, which gives a picture of your long-term control.
You’ll need explicit, non-negotiable instructions from your surgeon or endocrinologist on adjusting your insulin or other diabetes medications. The plan will likely include steps like these:
It's not just diabetes medications we need to consider. A surprising number of common prescriptions, over-the-counter drugs, and even herbal supplements can interfere with surgery. They can affect everything from blood clotting and blood pressure to how you react to anesthesia.
Medications Often Paused Before Surgery:
Medications Often Continued:
Some medications are essential for keeping you stable and are too important to stop. These usually include blood pressure pills, anti-seizure drugs, and many heart medications. We’ll typically have you take these as scheduled on the morning of surgery, but with only a tiny sip of water.
Your pre-op appointment is where we’ll finalize everything. We will sit down and create a definitive list of what to stop, what to continue, and the exact timing for each. This conversation is your most powerful tool for ensuring a safe and successful outcome.
Think of this guide as a detailed roadmap for your pre-surgery nutrition. But when it comes down to it, your surgical team's instructions are the only ones that matter for your procedure. Their orders are your personal, non-negotiable GPS route to a safe and successful outcome.
No two patients, surgeries, or medical facilities are exactly alike. The instructions you receive aren't just a generic handout; they're a safety plan carefully crafted just for you, which is why your friend might have gotten completely different advice for their procedure. This personalization is critical, as many factors can change the standard fasting rules.
The guidance you get is a mix of science, experience, and your personal health story.
Your instructions will be influenced by:
Medical guidelines are constantly being updated as new research gives us a clearer picture of what’s safest. While the "2/6 hour rule" is a widely accepted standard, some advanced surgical centers are moving to more flexible protocols backed by solid safety data.
This is another huge reason to stick to what your hospital tells you—they may be at the forefront of these changes.
For example, a major quality improvement project looking at over 653,000 cases found that allowing clear fluids up to one hour before anesthesia led to zero increase in aspiration events. While this is fantastic news for patient comfort, it’s a protocol that only your specific surgical facility can clear you for. You can dive deeper into these evolving guidelines over at RonLitman.Substack.com.
Here at Cape Cod Plastic Surgery, Dr. Fater and our anesthesia team provide every patient with precise, written instructions. We base our guidelines on the latest safety standards and your individual health profile to ensure you have the best possible experience.
Being an active partner in your surgical prep is the best way to feel confident and ready. Don't ever hesitate to ask questions until you feel 100% clear on the plan.
Here’s a final checklist of questions to run by your doctor:
Your surgeon’s office is there to help you. Writing down the answers gives you a simple, easy-to-follow game plan, which helps erase any last-minute stress and ensures you arrive for your surgery safely and confidently.
Even with a detailed guide, a few specific questions always seem to pop up. Those small, nagging uncertainties can create a lot of unnecessary stress, so let's clear them up right now. Think of this as your quick-reference guide for those last-minute "what ifs."
Getting these details sorted out will help you walk into your surgery feeling confident and calm, knowing you've done everything right.
This is probably one of the most-asked questions we get, and the short answer is no. Most anesthesiologists will tell you to skip the gum and hard candies on the morning of your procedure.
But why? Chewing gum or sucking on a mint gets your salivary glands working overtime. That means you swallow more saliva and air, increasing the fluid in your stomach. While the risk is small, it technically goes against the goal of having an empty stomach. It’s always best to play it safe and just avoid them.
Life happens. If you slip up and eat or drink something when you weren't supposed to, the most important thing to do is be honest. You must tell the pre-op nurse or your anesthesiologist the moment you get to the hospital or surgical center.
Please don't hide it. This is purely about your safety. Telling the team what you had and when allows them to make the safest decision. Your surgery may need to be delayed or rescheduled, which isn't a penalty—it's a crucial precaution to prevent dangerous complications while you're under anesthesia.
This one trips a lot of people up. Black coffee gets the green light as a clear liquid, but the second you add a splash of milk, cream, or even a dairy-free substitute, it changes the game.
The fats and proteins in milk and creamers turn your coffee into what your stomach treats as a "light meal." It simply won't digest as quickly as a true clear liquid. That’s why any coffee with add-ins needs to be finished at least six hours before your surgery, following the same rule as solid food.
Nope. Even if a drink is see-through, if it has protein in it, it's not a clear liquid in the eyes of an anesthesiologist. Protein slows down stomach emptying, which is exactly what we’re trying to avoid with fasting.
Stick with simple sports drinks like Gatorade or Powerade, which get their fuel from sugar and electrolytes. Just be sure to avoid any of the "enhanced" versions with added protein. When in doubt, read the label—or better yet, just stick to the approved list from your surgical team.
At Cape Cod Plastic Surgery, we believe a well-prepared patient is a calm patient. Dr. Fater and our entire team are committed to making sure you have all the information you need. If any other questions come to mind, please don't hesitate to ask. To learn more about our patient-first philosophy for cosmetic and reconstructive surgery, we invite you to visit our website.

February 21, 2026
Discover how to prevent keloid scars after surgery with our definitive guide. Learn expert strategies for risk assessment, surgery, and post-op scar care.

February 20, 2026
What is Ultherapy treatment? Explore this non-surgical facelift, how it uses ultrasound to lift skin, and what results you can expect from the procedure.

February 19, 2026
Explore stunning cheek filler before and after results. See real patient photos, learn about filler types, and discover what's possible for your facial contour.