
February 21, 2026
How to Prevent Keloid Scars After Surgery A Definitive Guide
Discover how to prevent keloid scars after surgery with our definitive guide. Learn expert strategies for risk assessment, surgery, and post-op scar care.
Feb 21, 2026

When it comes to preventing keloid scars after surgery, the best defense is a good offense. This isn't about just one thing; it's a dedicated plan that starts well before your procedure and continues for many months afterward. Think of it as a partnership between you and your surgeon, where we combine your personal risk factors, the latest surgical techniques, and a consistent aftercare routine to give your skin the best possible chance to heal beautifully.
It's a truth we see every day in our practice: preventing a keloid is much easier than treating one. There’s no single magic bullet. Instead, successful prevention is all about teamwork and understanding the "why" behind each step. Here at Cape Cod Plastic Surgery, we find that when our patients are empowered with knowledge, they become active participants in their own healing, leading to much better outcomes.
This whole process really boils down to three core areas: understanding your unique risks, the surgeon’s work in the operating room, and your commitment to the healing process at home.

To make this simple and actionable, we organize our keloid prevention strategy around three key pillars. Each one covers a different phase of your surgical journey, building a strong defense against unwanted scar tissue, particularly for those of us who know we're prone to it.
Here’s a quick overview of how these pillars work together to protect your skin.
By addressing each of these areas, we create a comprehensive plan that leaves as little as possible to chance.
The most crucial takeaway is that keloid prevention is not passive. It is an active process that requires awareness and consistency from both the patient and the surgical team to achieve the desired result.
This framework ensures every angle is covered. Of course, the quality of the surgery itself is a massive factor, which is why your choice of surgeon is so critical. A surgeon's skill directly impacts how your scar begins its healing journey. You can learn more about what to look for in our guide on how to choose a surgeon.
Now, let's dive deeper into each of these pillars. In the following sections, we’ll break down the specific, practical steps you can take to feel confident and in control of your recovery.
When it comes to scarring, not all skin is created equal. The very first step in preventing a keloid is to get a realistic sense of your personal risk. This isn't about causing anxiety; it's about being smart and proactive. Knowing your risk profile from the start allows us to build a more aggressive, targeted plan to manage your healing right out of the gate.
It's a bit like knowing you have sensitive skin—you wouldn't just use any random product. You'd choose carefully. In the same way, if we know your skin is prone to keloids, we can be much more deliberate with our prevention strategy.

Your genetic makeup is, by far, one of the most powerful predictors for keloids. These aggressive scars aren't just a fluke of healing; they have a strong hereditary link. If your parents or a sibling has a history of them, your own risk goes up significantly.
Ethnicity is also a major factor. While anyone can get a keloid, the incidence is much higher in people with more melanin in their skin.
This all comes down to how your body's fibroblasts—the little collagen factories in your skin—react to an injury. In people prone to keloids, these cells simply don't get the message to stop, churning out far more collagen than necessary to close a wound.
Your skin's past behavior is the best crystal ball we have for its future. Have you ever had a thick, raised, or itchy scar from a cut, piercing, or previous surgery? That’s a huge red flag. Even a tiny keloid from an ear piercing ten years ago gives us vital information for planning your procedure today.
Age plays a role, too. Keloids are most common in people under 30. This is likely because younger skin has a more vigorous, high-octane healing response, and that powerful engine can sometimes go into overdrive.
Frankly, your personal scarring history is a non-negotiable part of our conversation. It’s the single most reliable predictor of how your skin will handle a new incision.
Finally, where you have surgery matters. A lot. Certain parts of the body are notorious keloid hotspots, primarily because the skin in these areas is under constant tension from everyday movement. This continuous pulling and stretching can provoke that over-the-top healing response.
High-Risk Anatomical Zones:
By putting all these pieces together—genetics, personal history, age, and the surgical site—we can shift from a generic "wait and see" mindset to a truly customized plan. If a patient walks in with multiple risk factors, we know on day one that we need to bring out our most effective preventative tools immediately after their surgery.
While we have many tools to manage scars after surgery, your best defense against a keloid begins the moment the first incision is made. What happens in the operating room is foundational. The way a surgeon handles your tissue—how it's cut, managed, and closed—profoundly influences how it heals.
A keloid is essentially a healing process that's gone into overdrive. The surgeon's job, then, is to keep the entire procedure as gentle and non-traumatic as possible. Think of it like a master tailor working with delicate fabric. A careful cut and precise stitches create a flat, seamless result. But a rough, stretched, and poorly sewn seam will pucker and bunch. Your skin is no different.
It really all boils down to one critical factor: skin tension. Tension is the arch-nemesis of a calm, flat scar. When the edges of a wound are pulled tight, it's a blaring alarm for your body to send in the troops—in this case, an army of collagen-producing cells—to fortify what it perceives as a weak spot. For someone prone to keloids, that alarm is deafening, leading to a dramatic overproduction of scar tissue.
A skilled surgeon’s technique is all about outsmarting that overzealous healing response. It’s more than just having a steady hand; it's a strategic approach from start to finish.
By making these techniques our priority, we create a calm, stable environment for the wound. We're essentially sending signals to your body to heal normally, not to panic and overproduce collagen.
For anyone with a history of keloids, meticulous surgical technique is just the beginning. Relying on surgery alone is, frankly, setting ourselves up for failure. The data is sobering: recurrence rates for keloids after simple surgical removal can be anywhere from 45% to a staggering 100%.
In fact, without any follow-up treatments, about 70% of patients see their keloids return. These numbers aren't just statistics; they represent real frustration for patients and are the reason modern prevention strategies are so much more comprehensive. You can read the research behind these keloid recurrence findings to see the data for yourself.
This is where we bring in adjuvant therapies—treatments we use in combination with surgery to suppress that overactive healing process right from the get-go.
Think of it as a one-two punch. The surgeon skillfully removes the keloid and creates a beautiful, low-tension closure. Then, we immediately follow up with a treatment designed to calm the cellular response before it even has a chance to ramp up.
One of our most trusted and effective adjuvant treatments is the strategic injection of corticosteroids. These aren't the anabolic steroids you hear about in sports; they are powerful anti-inflammatory medicines that work wonders at the cellular level to keep healing in check.
Here’s how they work:
Timing is everything with these injections. We often give the first dose right there in the operating room, injecting it directly into the wound edges before we even place the final skin stitches. This gets the medicine exactly where it needs to be, right from day one.
From there, we typically schedule follow-up injections every few weeks for several months. This allows us to actively manage the healing process during its most critical phase, turning scar management from a reactive guessing game into a proactive, controlled strategy. It’s this combined approach that gives you the absolute best odds for a smooth, flat, and final result.
What we do in the operating room is just the beginning. Your commitment to scar care in the weeks and months that follow is what truly makes or breaks the final result. Think of it as an active partnership where consistency is everything. This is your game plan for navigating the healing process and keeping keloid scars at bay.
The first 48 hours are all about letting the incision heal in a quiet, undisturbed environment. We apply a specific dressing to keep the area clean and minimize swelling. During this initial window, your only job is to follow our instructions to the letter—usually just some gentle cleansing while avoiding any stretching or tension on the site. If you need a refresher, our detailed guide on how to properly care for surgical incisions is always available.
This timeline gives you a bird's-eye view of how our prevention strategy unfolds, layering different interventions together from the day of surgery through the critical early healing phase.
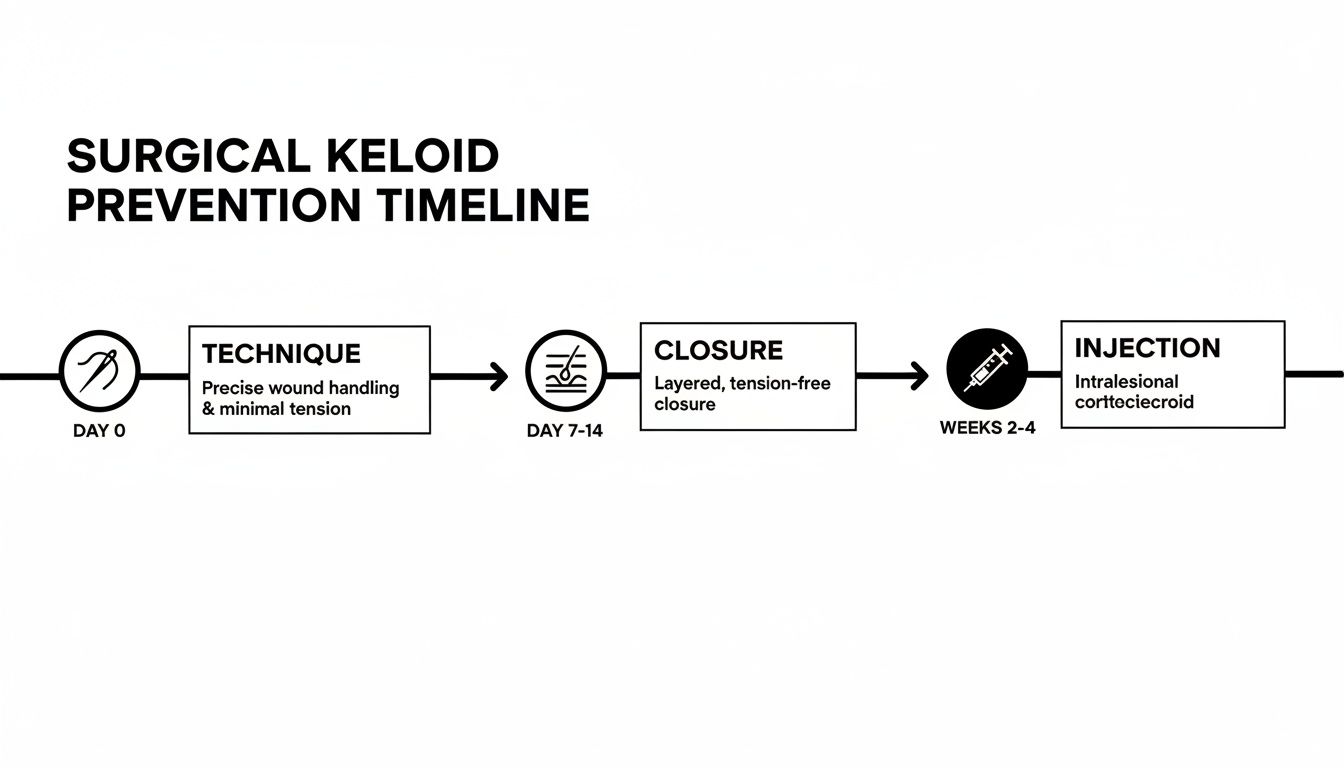
As you can see, preventing keloids isn’t a single action but a carefully timed sequence of events, starting with the surgical closure itself and followed by proactive treatments in the weeks that follow.
Once the initial healing is done and your sutures are out (typically around the 1-2 week mark), we shift gears to the cornerstone of long-term scar management: silicone. This isn't just a feel-good cream; it's a powerful, medical-grade treatment with a ton of clinical evidence showing how well it prevents angry, overgrown scars.
So, how does it work? Silicone creates a breathable, flexible shield over your scar that mimics the properties of healthy skin. This locks in moisture, creating an optimally hydrated environment.
That hydration is key. It sends a signal to your fibroblasts—the tiny collagen factories in your skin—to calm down. In essence, it tells them, "We're good here, no need to keep sending in the construction crew." This helps normalize collagen production and prevents that massive overgrowth that becomes a keloid.
Think of silicone sheeting as a personal trainer for your healing scar. It applies gentle pressure and creates the perfect environment to encourage disciplined, orderly healing rather than chaotic overgrowth.
For this to work, you have to be diligent. We have our patients use silicone gel or sheets for 12-24 hours a day. This consistency is absolutely vital, especially during the first three to six months when the scar is most active and vulnerable. It’s a marathon, not a sprint.
Working hand-in-hand with silicone, pressure therapy is another fantastic tool, especially for high-risk areas. The idea is simple: apply constant, gentle pressure directly onto the healing scar. This sustained pressure is believed to reduce blood flow just enough to limit the oxygen and nutrients that fuel those overzealous collagen-producing cells.
But this isn't a one-size-fits-all approach. The method has to be tailored to the specific surgery site.
The secret to pressure therapy is that it must be continuous. Just like silicone, it demands daily wear for several months to be effective. For many of our patients, we'll recommend a combination approach, using both silicone sheets and a pressure garment. This dual strategy creates the most robust defense possible against keloid formation.
When we’re dealing with a very high risk of keloid recurrence—perhaps because of a strong family history or scars that have stubbornly returned after previous treatments—we have to pull out the big guns. For these specific cases, just using silicone sheets and pressure dressings isn’t going to be enough. This is where we bring in one of our most effective tools: Superficial Radiation Therapy (SRT).
I know the word "radiation" can sound a little scary, but it's crucial to understand that SRT is nothing like the high-dose radiation used for cancer. This is a very low-energy therapy that only penetrates a few millimeters deep into the skin. Its entire job is to target the overactive fibroblast cells that go into overdrive and produce way too much collagen after surgery. By delivering a precise, controlled dose of radiation, we can essentially tell those cells to calm down before they even get started.
For someone facing a high likelihood of keloid formation, preventing another one from appearing becomes a long-term commitment, much like mastering chronic condition management at home. It takes a dedicated, proactive mindset, and SRT is a cornerstone of that intensive plan.
Here’s the most important thing to know about SRT: its success is almost entirely about timing. The therapy works best when we use it during the body’s initial, most aggressive phase of wound healing.
Ideally, we need to start the first session within 24 to 48 hours after your keloid removal surgery.
This narrow window is non-negotiable. If we wait even a week, the fibroblasts have already multiplied and started their runaway collagen production, and the treatment becomes far less effective. By getting in there right away, we intercept the process at its source, calming the healing response before it has a chance to get out of hand.
A typical SRT plan involves a series of quick, easy treatments.
To make this happen, we work hand-in-hand with a radiation oncologist. Your surgical appointment and your first SRT session are scheduled together as a single, coordinated plan to ensure everything is seamless.
Modern SRT is incredibly safe and targeted, with a proven track record for keloid prevention that goes back decades. Because the therapy is so superficial, the radiation stays within the scar tissue itself, protecting all the healthy surrounding skin and any underlying organs.
And the results? They speak for themselves. The research is clear: combining surgery with post-op SRT gives us one of the highest success rates for stopping keloids from coming back. Studies have shown exceptionally low regrowth rates when the therapy is timed and dosed correctly. A major retrospective study found SRT had cure rates of 85.6 percent from 24 months onward.
The data further shows that when surgery is paired with this kind of adjuvant radiotherapy, recurrence rates can plummet to as low as 0 to 8.6 percent. That’s a massive improvement over the nearly 70 percent recurrence rate we often see with surgery alone.
The most common side effect is a temporary change in skin color right at the treatment site. Some people might notice the area gets a bit lighter or darker, but this usually fades over time. Importantly, long-term studies have confirmed an excellent safety profile.
This advanced therapy is a vital part of our tiered approach to keloid management. It gives our highest-risk patients a truly reliable and powerful option to finally break the cycle of recurrence. While not everyone needs this level of intervention, knowing it’s available brings a lot of peace of mind. For other skin health and scar management needs, different advanced treatments, like those we cover in our post on the benefits of microneedling with PRP, can also be excellent options.
After surgery, your focus naturally shifts to healing well and getting the best possible result. If you're prone to keloids, you probably have a lot of specific questions about what comes next. We get it. Feeling confident in your aftercare plan is a huge part of the process.
Let's walk through some of the questions we hear most often in our practice. Our goal is to give you clear, practical answers so you know exactly what to do.
This is one of the first things patients ask, and it's a great question. The short answer is: longer than you might think. Keloid prevention is a marathon, not a sprint. A scar might look healed on the surface within a few weeks, but the remodeling process happening underneath the skin can take a full year, sometimes even longer.
We typically have our patients stick with a dedicated scar care routine for at least 6 to 12 months. The first few months are absolutely critical—that's when the scar is most active and we have the biggest opportunity to influence how it heals. Consistent use of medical-grade silicone sheets or gel during this period is essential. As we see you for follow-ups, we’ll be checking the scar’s progress and will let you know when you can start to ease up on your routine.
My best advice is to think of that first year as your make-or-break window. The diligence you show now is what will lead to a flat, subtle scar down the road.
Knowing what to look for is your best defense. If you can spot the early signs of a problem, we can step in and act quickly, which is when our treatments are most effective. A normal healing incision will be a little pink and firm at first, but certain changes should get your attention.
Keep an eye out for these specific red flags:
Catching these changes early makes all the difference. A timely steroid injection can stop a budding keloid in its tracks, which is far easier and more effective than trying to tackle a large, mature scar months later.
You've probably seen them at the pharmacy—tubes and jars of creams promising to make scars vanish. While many of these products, like those with onion extract (Mederma) or vitamin E, are popular, there isn’t much solid scientific evidence to show they prevent keloids.
When it comes to preventing tough, overgrown scars, the only topical treatment with decades of robust clinical research behind it is medical-grade silicone. It works by creating a breathable, flexible seal over the scar, which locks in moisture. This hydrated environment helps calm down the cells that produce collagen, encouraging them to remodel the scar in an orderly way instead of going into overdrive.
For our patients, especially anyone with a history of keloids, we stick to what’s proven. We'll always recommend medical-grade silicone gel or sheets because they give you the most reliable shot at a smooth, flat scar. We'll even point you to the specific products we trust and show you exactly how to use them.
At Cape Cod Plastic Surgery, our commitment to you doesn't end when you leave the operating room. We're with you for every step of the healing journey. If you ever have a concern about how your scar is healing or want to create a personalized prevention plan, we are here to help. Contact us today to schedule your consultation.

February 21, 2026
Discover how to prevent keloid scars after surgery with our definitive guide. Learn expert strategies for risk assessment, surgery, and post-op scar care.

February 20, 2026
What is Ultherapy treatment? Explore this non-surgical facelift, how it uses ultrasound to lift skin, and what results you can expect from the procedure.

February 19, 2026
Explore stunning cheek filler before and after results. See real patient photos, learn about filler types, and discover what's possible for your facial contour.