
February 21, 2026
How to Prevent Keloid Scars After Surgery A Definitive Guide
Discover how to prevent keloid scars after surgery with our definitive guide. Learn expert strategies for risk assessment, surgery, and post-op scar care.
Nov 14, 2025
A mastectomy is a profound experience, and the choices that follow are deeply personal. When it comes to breast reconstruction, the path forward generally splits into two main directions: using breast implants (either saline or silicone) or using your own natural tissue in a procedure known as autologous reconstruction.
The right decision for you will come down to a thoughtful conversation about your health, your cancer treatment plan, and what you hope to achieve.
Embarking on breast reconstruction is a significant step toward restoring your body and feeling whole again. Think of it not as a single surgery but as a collaborative journey with your breast surgeon and your plastic surgeon. The ultimate goal is to craft a plan that fits your body, your lifestyle, and your aesthetic goals. This guide is designed to walk you through all the available choices, giving you the clarity needed to make confident decisions.
As you start this process, the first big things to understand are the foundational approaches and the timing. These initial decisions will shape your entire reconstructive experience.
Getting familiar with the main pathways is your first step. You and your surgical team will weigh several critical factors to map out the best approach for your unique situation.
Demand for these procedures is on the rise, thanks to surgical advances that deliver more natural-looking results than ever before. In fact, breast reconstruction surgeries jumped by 31% between 2020 and 2021 alone, a number that reflects both rising breast cancer rates and vastly improved techniques.
As you explore these options, it can be helpful to learn more about what is reconstructive surgery in a broader sense. It's also wise to consider the wider implications of cancer treatment; for example, learning about the impact of breast cancer drugs like Tamoxifen on fertility can be incredibly insightful for future family planning.
When it comes to breast reconstruction after a mastectomy, your options really boil down to two main paths. The first, and most common approach in the U.S., is implant-based reconstruction. This involves using either saline or silicone implants to create a new breast shape.
The second path is autologous reconstruction, which you might hear called "flap surgery." This is a more advanced technique where a surgeon uses your own body tissue—usually a combination of skin, fat, and sometimes muscle from another area like your belly or back—to build a soft, natural-feeling breast. Each journey has its own timeline, recovery experience, and final look.
This visual guide breaks down the fundamental choices you'll face, from the materials used to the timing of the surgery itself.
Think of these as the building blocks of your reconstruction plan: will you use implants or your own tissue, and when will the surgery happen?
For many women, implant-based reconstruction isn't a single operation but a staged process. It typically starts with placing a tissue expander—a sort of empty, temporary implant—under the chest muscle during the mastectomy. Over the next few months, you'll visit your surgeon’s office to have this expander gradually filled with saline, which gently stretches the skin to create a pocket for the final implant.
After the skin has stretched enough, a second, shorter surgery is scheduled to remove the expander and put the permanent saline or silicone implant in its place. Some women, often those with smaller breasts or enough healthy skin left after mastectomy, might be able to skip the expander step and go straight to a direct-to-implant procedure.
The biggest draw for implants is a less demanding initial surgery. Recovery is quicker, and you won't have scars on other parts of your body. The trade-off, however, is that implants aren't forever. They will likely need to be replaced or revised down the road.
Autologous reconstruction, or "flap" surgery, works from a completely different philosophy. Instead of an implant, your surgeon essentially transplants a section of your own skin, fat, and its blood supply (the "flap") from a donor site to create a new breast. It’s a bit like an intricate sculpting process using your own materials.
The lower abdomen is the most common donor site, which gives the added cosmetic perk of a "tummy tuck." But tissue can also be taken from the back, thighs, or buttocks. Because the new breast is made from your own living tissue, it tends to feel softer and move more naturally. It will also change with you as your weight fluctuates over time, just like a natural breast.
To really get a handle on these two paths, it helps to see their core differences laid out side-by-side. Remember, this isn't about which one is "better" in general, but which one is the right fit for your body, your health, and what you want to achieve.
Ultimately, this table highlights the fundamental trade-offs: implants offer a simpler, faster initial recovery, while autologous reconstruction provides a more natural and permanent result at the cost of a more complex surgery.
When it comes to breast reconstruction after a mastectomy, implants are a familiar and often-chosen path. This approach uses either saline or silicone devices to build a new breast mound, offering a way back to form and symmetry with less surgical complexity than options that use your own body tissue.
Their popularity is reflected in the numbers. The global market for these devices was valued at around USD 2.5 billion back in 2025 and is projected to more than double by 2035. A big part of this growth comes from innovations that create more natural-looking results, with smaller implants now making up over 26.7% of the market. If you want to dive deeper into the data, you can read the full analysis on the mastectomy reconstruction implants market.
Many women lean toward implants because the initial surgery is shorter and the recovery is faster, which can be a huge relief during an already stressful time. But it's important to understand that this is a journey with its own set of considerations, from the type of implant you select to the long-term care you'll need.
For most women, implant reconstruction happens in two distinct phases. This staged approach is designed to give your body time to prepare for the final implant.
In certain situations, a direct-to-implant procedure is an option. This is a single-stage surgery where the final implant is placed at the same time as the mastectomy. This is generally reserved for women with smaller breasts or those who have enough healthy, pliable skin left after the mastectomy to safely cover the implant without needing to stretch the tissue first.
Choosing between saline and silicone is a major decision, as each type has a different feel, appearance, and requirement for long-term monitoring.
Silicone Implants
These implants come pre-filled with a cohesive silicone gel that does a remarkable job of mimicking the feel of natural breast tissue. For this reason, they are often the preferred choice for women who want a softer, more natural texture and want to minimize the risk of visible rippling under the skin.
Saline Implants
Saline implants have a silicone outer shell but are filled with a sterile saltwater solution. They're put in empty and then filled during surgery, which gives the surgeon a little flexibility to fine-tune the size.
While both implant types have an equal chance of rupture, the key difference lies in detection and monitoring. Silicone requires proactive surveillance, whereas a saline rupture is self-evident, simplifying the follow-up process but requiring prompt surgical attention.
Opting for implant reconstruction is a long-term commitment. Unlike reconstructions using your own tissue, which become a permanent part of you, implants are medical devices. They don't last forever. Most have a lifespan of about 10 to 15 years, which means that future surgeries aren't just a possibility—they're a probability.
One of the most common long-term complications is capsular contracture. This happens when the scar tissue that naturally forms around any implant tightens and squeezes it. This can make the breast feel hard, look distorted, and sometimes become painful. In fact, it's the number one reason women with implants need a reoperation.
Other future surgeries might include:
Ultimately, implant-based reconstruction offers a more straightforward surgical path with a quicker initial recovery. It’s an excellent choice for women who prefer a less invasive procedure and want to avoid scars on other parts of their body. The trade-off, however, is the need for ongoing vigilance and the high likelihood of more surgeries down the road to maintain your results.
For many women, the most natural-feeling path to reconstruction after a mastectomy is using their own body tissue. This approach, known as autologous or "flap" reconstruction, is a more complex surgical journey, but the outcome is a soft, warm breast that feels and ages just like the real thing.
It's a world away from implants. Instead of a synthetic device, your surgeon transfers a section of skin, fat, and its own blood supply—the "flap"—from another part of your body to your chest. It's a delicate process that leans heavily on microsurgery to meticulously reconnect tiny blood vessels, making sure the transplanted tissue gets the circulation it needs to thrive.
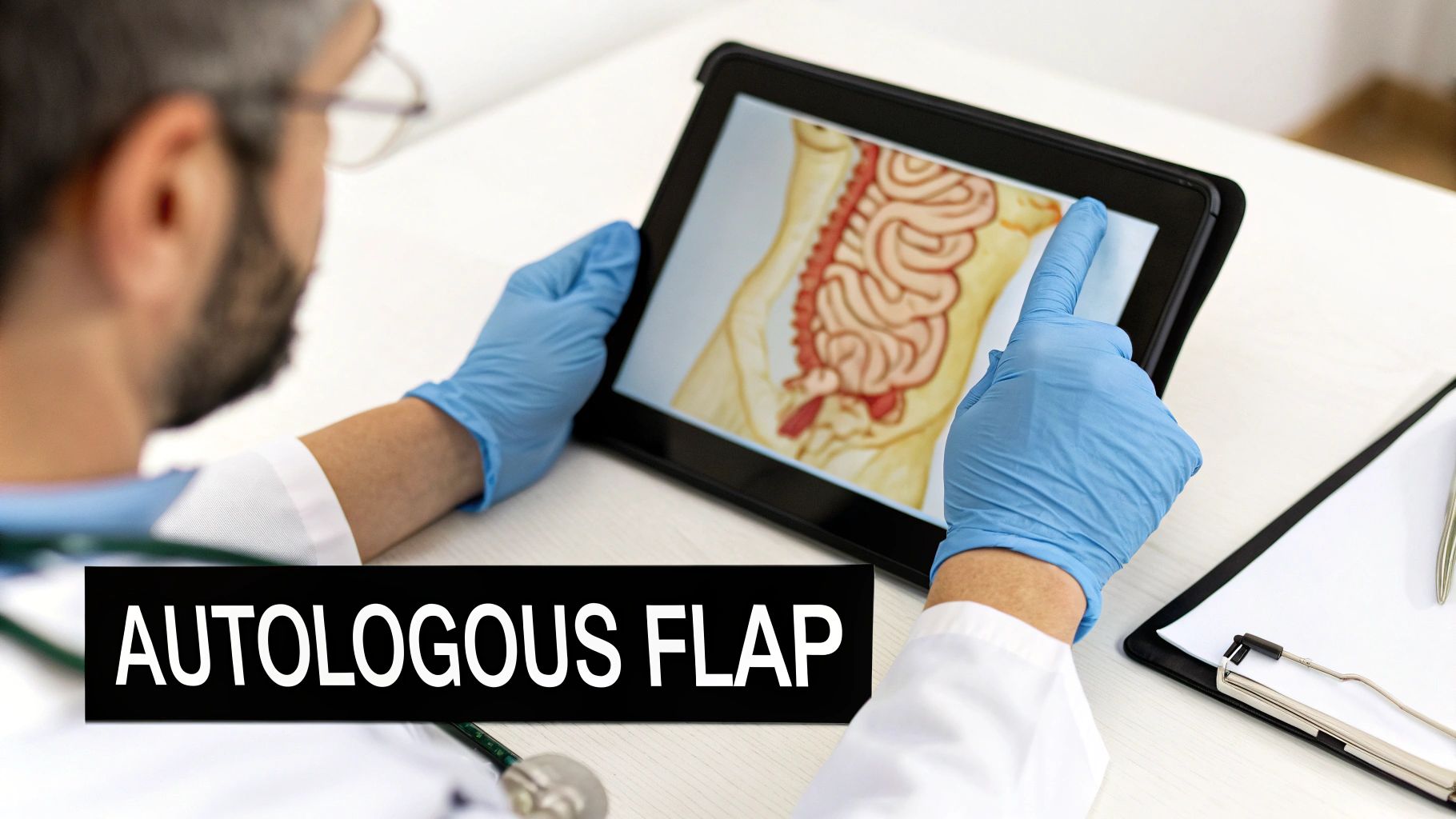
Many consider this the gold standard for a reason. The new breast will gain or lose weight with you and settle naturally over time, just like a natural breast would. This creates a lasting symmetry that you won't have to worry about down the road.
The lower abdomen is the most popular donor site, hands down. It usually has enough extra tissue to create a beautifully shaped breast, and as a bonus, it gives you a flatter stomach—much like a tummy tuck. When using abdominal tissue, the two main procedures are the DIEP and TRAM flaps.
DIEP (Deep Inferior Epigastric Perforator) Flap
The DIEP flap is the modern workhorse of breast reconstruction. Surgeons painstakingly isolate tiny blood vessels (perforators) that travel through the abdominal muscle, taking only the necessary skin and fat. The game-changer here is that the rectus abdominis muscle is left almost entirely intact.
TRAM (Transverse Rectus Abdominis Myocutaneous) Flap
The TRAM flap is an older technique that also uses tissue from the lower belly. The key difference is that instead of just taking the blood vessels, it moves a portion (or sometimes all) of the rectus abdominis muscle along with the skin and fat. That muscle acts as the built-in life support system, carrying the blood supply to the flap.
The real story here is muscle preservation. A DIEP flap is all about maintaining your core strength by leaving the muscle behind. A TRAM flap sacrifices some of that muscle to get the job done. For that reason, the DIEP flap has become the clear favorite whenever it’s an option.
Not everyone has enough extra tissue on their abdomen or is a candidate for that type of surgery. If you're very lean or have had previous surgeries like a tummy tuck, don't worry. Your surgeon has other excellent breast reconstruction options after mastectomy to consider.
These alternatives still rely on sophisticated microsurgical skills and deliver that same natural, permanent result.
Deciding on an autologous flap reconstruction is a major step. It means a longer surgery and a more involved initial recovery. But the payoff is immense: a living, breathing part of you that never needs to be replaced and will feel like your own for the rest of your life.
Once you've considered implants versus your own tissue, the next big question is when to have the reconstruction. This isn't just about scheduling; the timing of your surgery shapes everything from the surgical plan itself to your physical and emotional recovery journey. Your decision will be closely tied to your overall cancer treatment, especially if radiation therapy is part of the plan.
There are really two main paths for the different breast reconstruction options after mastectomy: immediate or delayed. Each has its own rhythm and is suited for different medical situations and personal preferences. Getting this piece right is crucial for a reconstruction plan that truly supports your healing and gives you peace of mind.
Immediate reconstruction is exactly what it sounds like—we begin rebuilding your breast in the same operation as your mastectomy. The biggest benefit here is often psychological. You wake up from surgery with a breast mound already there, which can soften the emotional impact of seeing a flat chest. It also consolidates two major procedures into one, meaning you only have one big recovery period to navigate.
This all-in-one approach is a popular choice for its efficiency and positive emotional effect. In fact, rates for immediate breast reconstruction have leveled out at around 32.7% of all mastectomy patients, showing how many women value this option for their psychological well-being. If you're interested in the data, you can explore the research on reconstruction rates stabilization to see these trends.
This path is typically a great fit for women who won't need radiation therapy after their mastectomy.
The real power of immediate reconstruction is the sense of continuity it provides. It helps bridge the gap between the mastectomy and feeling whole again, allowing you to start your emotional healing right away.
Delayed reconstruction happens months, or sometimes even years, after your mastectomy and all cancer treatments are finished. I know waiting can sound difficult, but it's often the safest and smartest medical decision, especially if you need radiation.
Radiation therapy dramatically changes the skin and tissues on your chest. They become tighter, less elastic, and have a reduced blood supply. Trying to place an implant or even tissue flap into that environment right away is asking for trouble. It significantly raises the risk of complications, such as:
By waiting, you give your body time to completely heal from both the surgery and the radiation. Once that tissue has recovered and stabilized, your surgeon has a much healthier and more predictable canvas to work with. This leads to a better long-term cosmetic result with far fewer headaches. It also lets you focus 100% on your cancer treatment without the extra stress of a concurrent reconstruction recovery. Planning is key, and our guide on how to prepare for surgery offers practical advice for any procedure you're facing.
Ultimately, deciding on the timing is a team sport. You'll make this choice alongside your breast surgeon, oncologist, and plastic surgeon. It's about striking the right balance between your medical needs, what you feel ready for, and the path that will give you the best, most beautiful, and lasting result for your new beginning.
Navigating the world of breast reconstruction options after mastectomy is an intensely personal journey. There’s no universal "best" choice here—only what's right for your body, your health, your lifestyle, and your personal goals. It's easy to feel overwhelmed by all the information, but breaking it down can help you find clarity and move forward with confidence.
Start by thinking about what's truly most important to you. Are you looking for a shorter, more straightforward initial recovery, or is a completely natural, long-lasting result worth a more involved surgical process? Your own body and overall health play a huge role, too. For example, if you have enough tissue in your abdominal area, you might be an ideal candidate for a DIEP flap. If you have a leaner frame, implants might be a more practical route.

The consultation with your plastic surgeon is where everything starts to come together. This is your time to get answers, so arriving prepared with a list of questions will make the conversation incredibly productive.
Think about asking things like:
Your final plan is a collaborative effort. It’s a partnership between you and your medical team, where your personal values and your surgeon's expertise come together to create a result that enhances your quality of life.
The skill and experience of your surgeon are absolutely crucial in this process. If you need help with this step, our guide on finding a plastic surgeon can point you in the right direction.
Remember, every path is valid—whether it involves multiple stages, nipple reconstruction, or choosing to "go flat." The only outcome that matters is the one that feels right for you, honoring your body and supporting your journey to wholeness.
Going through the details of breast reconstruction naturally brings up a lot of questions. We’ve found that patients often have similar concerns, so let's walk through some of the most common ones to give you a clearer picture of what to expect.
This is one of the most important questions we discuss. The honest answer is that a reconstructed breast will not feel the same as your natural breast. During a mastectomy, the nerves that give you sensation are cut, which means feeling in the breast and nipple is lost.
While the shape and appearance can be wonderfully restored, the function—including sensation—is not. Some patients notice a bit of surface feeling return over time, sometimes years later, but it’s not the deep, natural sensation you were used to. Newer nerve-grafting techniques are being developed, but they aren't widely available yet. It’s best to go into this process with realistic expectations about what can and can't be restored.
A reconstructed breast is meant to restore your silhouette and help you feel whole again, but it's important to understand it won't restore natural sensation.
Radiation is a real game-changer when it comes to planning a reconstruction. The therapy is incredibly effective at treating cancer, but it does leave its mark on the skin and underlying tissues. It can make them less flexible and reduce blood flow, which creates a more challenging environment for healing.
For this reason, if radiation is part of your plan, an immediate implant-based reconstruction is often not the best first step. The risk of complications like capsular contracture—where the scar tissue around the implant becomes painfully hard—or even implant failure is much higher in radiated tissue. Many surgeons will recommend waiting until after radiation is complete (a delayed reconstruction) and often suggest using your own tissue (an autologous flap), as it brings a fresh, healthy blood supply to the area, leading to a more predictable and lasting result.
Recovery time is a major factor in deciding which path is right for you, and it differs quite a bit between the two main approaches.
Knowing these timelines helps you plan your life around the surgery, arranging for the support you'll need and giving your body the dedicated time it requires to heal well.
At Cape Cod Plastic Surgery, Dr. Fater and our entire team are here to help you navigate these questions and make the best decisions for your body and your life. We believe in creating a personalized plan that helps you feel confident and whole again. Schedule a consultation to explore your options with us.

February 21, 2026
Discover how to prevent keloid scars after surgery with our definitive guide. Learn expert strategies for risk assessment, surgery, and post-op scar care.

February 20, 2026
What is Ultherapy treatment? Explore this non-surgical facelift, how it uses ultrasound to lift skin, and what results you can expect from the procedure.

February 19, 2026
Explore stunning cheek filler before and after results. See real patient photos, learn about filler types, and discover what's possible for your facial contour.