
February 21, 2026
How to Prevent Keloid Scars After Surgery A Definitive Guide
Discover how to prevent keloid scars after surgery with our definitive guide. Learn expert strategies for risk assessment, surgery, and post-op scar care.
Jan 2, 2026

The short answer is yes, insurance can cover plastic surgery. But it all comes down to one critical question: is it a medical necessity?
Think of it like car insurance. Your policy will pay to fix your bumper after a fender bender, but it won't cover that custom paint job you've been dreaming of. The same logic applies here—coverage hinges on whether the surgery is reconstructive (to restore function) or cosmetic (to enhance appearance).
To figure out if your procedure has a shot at being covered, you first need to understand the firm line insurance providers draw between cosmetic and reconstructive work. Their entire decision-making process is built around this distinction.
Reconstructive surgery is all about restoring normal function and appearance to parts of the body affected by things like birth defects, accidents, infections, or disease. Its job is to correct a medical problem and improve your quality of life.
Cosmetic surgery, on the other hand, is elective. It’s performed to reshape normal parts of the body simply to improve how they look. Since these procedures aren't medically required, they're almost never covered by insurance. This gap is a major reason why the U.S. saw over 6.1 million aesthetic procedures performed, with many patients paying entirely out of pocket.
Let's quickly break down the fundamental differences. This is exactly what your insurance company will be looking at when they review your case.
This simple table highlights the core motivation behind each type of surgery, which is the key to understanding your potential coverage.
At the end of the day, it all boils down to one simple question.
The fundamental question an insurer asks is: "Is this procedure needed to correct a functional problem, or is it desired to improve appearance?"
Your answer to that question is what truly determines whether you'll get coverage. If you'd like to learn more about the specifics, our detailed guide explains what reconstructive surgery is and the wide range of conditions it can address.

If there’s one phrase you need to understand when it comes to insurance and plastic surgery, it’s “medical necessity.” This is the magic key that can unlock coverage, but it's also where most people get tripped up. To an insurance company, this isn't a fuzzy concept; it's a hard-and-fast checklist they use to decide whether to approve or deny your claim.
Think of it like building a legal case. Your surgeon is your advocate, and your medical records are the body of evidence. Together, you have to prove, beyond a reasonable doubt, that this surgery isn't just about looking better—it's about living better by fixing a genuine functional problem.
Insurance companies operate on data and documentation. They need cold, hard facts—objective, verifiable proof that your procedure is meant to treat a diagnosed medical condition. Vague complaints about discomfort or simply wanting to improve your appearance just won't cut it.
Your job is to clearly connect the dots for them: show that a specific medical problem is causing a specific functional issue, and this surgery is the only effective solution. For instance, "I want a nose job" is a cosmetic desire. But, "My deviated septum is causing a 70% airway obstruction and chronic sinus infections" is a medical necessity. You can learn more about insurance coverage for a deviated septum in our detailed guide.
To build a compelling case, your insurer will expect to see some combination of the following:
Your plastic surgeon is your greatest partner in this whole process. They know what kind of language gets an insurer's attention and what evidence is needed to back it up. When you go in for a consultation, be ready to talk about the functional problems you're experiencing, not just your aesthetic wishes.
Let's take a breast reduction, for example.
Your case for medical necessity isn't built on wanting smaller breasts; it's built on providing evidence of chronic back pain, neck strain, skin irritation, and deep shoulder grooving from bra straps—all documented by a medical professional.
Your surgeon will take all this information and compile a detailed preauthorization request. This package is essentially your argument, laid out in the precise format insurance companies require, explaining why does insurance cover plastic surgery in your unique situation. They will frame the procedure as the logical next step in your medical treatment.
Ultimately, getting your procedure covered boils down to shifting the conversation from "want" to "need." It takes meticulous documentation and clear communication. By working closely with your surgeon, you can put together the strongest possible case to get the coverage you deserve.

While the words "plastic surgery" often bring to mind purely cosmetic changes, there are many procedures that insurance companies will cover—as long as there's a clear medical reason. The key is proving that the surgery is needed to restore function or relieve a physical problem, not just to change your appearance.
Success in getting these procedures approved almost always comes down to rock-solid documentation that lines up perfectly with your insurer's specific rules. Let’s walk through some of the most common procedures that get the green light when a strong case for medical necessity is made.
Breast reconstruction after a mastectomy is probably the most well-known example of a covered procedure. In fact, it's protected by federal law. The Women's Health and Cancer Rights Act of 1998 mandates that most health plans covering mastectomies must also cover the reconstruction process. This isn't just a single surgery; it often includes all stages needed to restore a natural look, including work on the other breast to create symmetry.
Breast reduction (reduction mammoplasty) can also get coverage, but you have to prove that oversized breasts (macromastia) are causing real physical harm.
Your doctor will need to document issues like:
To get approval, your surgeon has to build a case that the surgery is about relieving these symptoms, not just achieving a certain look. They'll submit your medical history, height, weight, and even the specific amount of tissue they plan to remove to make their point.
Blepharoplasty, or eyelid surgery, is a classic example of a procedure that can be either cosmetic or reconstructive. When it's done to get rid of droopy, excess skin that’s literally hanging in your line of sight, it’s considered medically necessary. This condition, known as ptosis or blepharochalasis, can seriously get in the way of your peripheral or upper vision.
For an insurer to say yes, you'll need objective proof. This usually means a trip to an ophthalmologist for a visual field test, which measures exactly how much your vision is blocked. Your surgeon will also take detailed photos to show the insurance company just how severe the drooping is.
Rhinoplasty to change the shape of your nose is almost always cosmetic. But surgeries to help you breathe better? Those are frequently covered. A septoplasty, which fixes a deviated septum, is the most common example. This procedure straightens the wall of cartilage and bone inside your nose, opening up the airway.
Your insurance might also cover other procedures like nasal valve repair or turbinate reduction if they're causing serious breathing issues. The trick is providing solid evidence, like notes from an Ear, Nose, and Throat (ENT) specialist or the results of a nasal endoscopy that confirms a structural problem.
After losing a massive amount of weight, many people are left with a large "apron" of excess skin and fat hanging from their lower abdomen. A panniculectomy is the surgery to remove this flap, known as the pannus. It's important to understand this isn't a tummy tuck (abdominoplasty), which also tightens the abdominal muscles for a flatter stomach. A panniculectomy focuses solely on removing the problematic skin.
Insurance will typically only cover this if the pannus is causing medical issues, such as:
On a related note, it's worth being cautious about seeking purely cosmetic procedures overseas. While your insurance won't cover the elective surgery itself, you might be surprised to learn who pays if things go wrong. A study of patients returning from "medical tourism" found that of those needing follow-up care for complications, 62% had their treatment covered by Massachusetts Medicaid and another 10% by Medicare. This highlights how public programs can end up footing the bill for adverse outcomes from cosmetic trips abroad. You can learn more about the findings on plastic surgery abroad.
Let's be clear: while some surgeries can walk the line between reconstructive and cosmetic, many are firmly planted in the "elective" camp. When a procedure is considered elective, insurance companies see it as a choice, not a medical need. That means you should expect to pay for it yourself.
Knowing which surgeries are almost always excluded from coverage helps you set realistic financial expectations right from the start. The logic insurance companies use is simple: if a procedure's main goal is to change or improve how you look, it's not considered medically necessary, and they won't cover the cost.
The following list includes some of the most popular aesthetic surgeries people choose today. These are all about reshaping, contouring, and rejuvenating your appearance—a personal investment in how you want to look, not a medical treatment.
You can pretty much count on these procedures not being covered by your insurance plan:
The bottom line is this: If the main reason for the surgery is to improve your appearance, you'll be paying for it. If the main reason is to improve your body's function, you've got a shot at coverage.
It’s more important than ever to understand these insurance rules, especially since aesthetic procedures are becoming incredibly popular. The demand for cosmetic surgery is soaring worldwide.
Globally, doctors performed nearly 38 million aesthetic procedures—both surgical and non-surgical—in a recent year. That’s a massive 42.5% jump over just four years. The United States is at the heart of this trend, accounting for over 6.1 million of those procedures. You can dig into the numbers yourself in the ISAPS Global Survey.
This boom shows that more and more people are willing to invest in themselves. When you're considering one of these popular but uncovered procedures, your focus shouldn't be on insurance battles. Instead, it's about smart financial planning and, most importantly, finding a board-certified surgeon you can trust. This is a personal investment, and you deserve a qualified expert who will deliver safe, beautiful results.
Let’s be honest: dealing with insurance can feel like trying to solve a puzzle in the dark. It’s a world of confusing forms, strict rules, and what seems like a language all its own. But when it comes to getting your reconstructive surgery covered, understanding the process is your most powerful tool.
The entire journey really boils down to one critical first step: preauthorization.
Think of it like getting a building permit before you start construction. You wouldn't just start digging a foundation without the city’s approval, right? Preauthorization—sometimes called prior authorization—is you and your surgeon formally asking the insurance company for a green light before the procedure happens. For any non-emergency reconstructive surgery, this isn’t just a good idea; it’s almost always required.
This is the insurance company’s chance to do a deep dive into your case. They’ll pore over your medical records, your surgeon's detailed notes, photos, and any test results to decide if your surgery meets their specific coverage criteria. Getting that "yes" at the preauthorization stage is the most important hurdle to clear.
While your surgeon's office will be the one to officially submit the request, the strength of that request depends entirely on the evidence you build together. A rock-solid preauthorization packet leaves no room for interpretation.
The goal is to paint a crystal-clear picture that your procedure is medically necessary—that it's meant to fix a functional problem, not just for cosmetic reasons. Every single document helps tell that story.
This is why your medical records are so important. Let's say you're seeking a breast reduction. Simply saying you have back pain won’t cut it. A strong case would include notes from your primary care doctor, proof that you’ve tried physical therapy, and even photos showing skin irritation or deep grooves in your shoulders from your bra straps. Each piece of evidence adds another layer of proof.
Even with a perfectly prepared packet, denials can happen. It’s incredibly frustrating, but a "no" is rarely the final word. Think of an initial denial as the start of a negotiation, not the end of the line. You have the right to appeal, and a surprising number of patients who fight back end up getting approved.
If you get that dreaded denial letter, don't panic. The next step is figuring out how to appeal a health insurance denial, which can make all the difference. The appeals system is there to give you another shot at making your case.
The process usually has two main levels:
This flowchart breaks down the four stages of a typical appeal, from the initial review to the final decision.
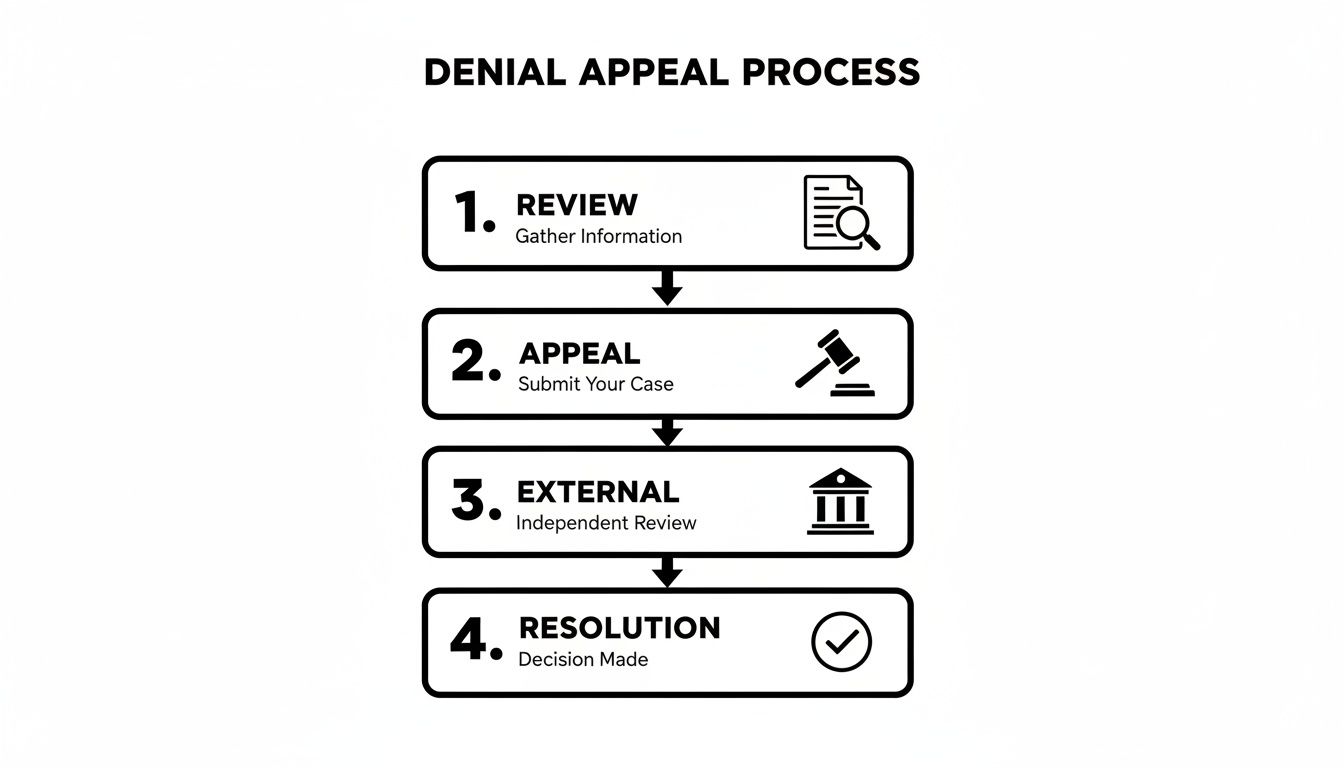
As you can see, a denial isn't a dead end. It’s just one step in a much larger process that can still lead to a successful outcome.
To win an appeal, you need to be organized and persistent. The secret is to directly address why the insurer denied your claim. Was there a paperwork error? Did they say you lacked sufficient proof? Your denial letter should spell out their exact reasoning.
Team up with your surgeon's office to gather any new information that can punch holes in their argument.
An appeal is often won with fresh, compelling evidence that wasn't in the original request. This could be a second opinion from another doctor, new test results, or a more detailed letter from your surgeon.
Make sure your appeal is in writing, and clearly explain why you believe their decision was wrong. Keep copies of everything and create a log of every phone call—note the date, time, and the name of the person you spoke with.
In this game, being proactive is your best strategy. By understanding how preauthorization and appeals work, you shift from being a passive patient to a powerful advocate for your own health.
Getting clear answers starts with asking the right questions. When you walk into a conversation with your surgeon or call your insurance company, being prepared is your best strategy. Think of it as doing your homework—it helps you understand your options and, most importantly, avoid frustrating surprises later on.
Vague questions often lead to vague answers. To get the specific, actionable information you need to make smart decisions about your health and finances, you need to be direct.
Your surgeon's office can be your biggest advocate in the insurance maze. Their team has likely been down this road many times before, so tap into that experience.
For a more complete checklist, take a look at our guide on questions to ask your cosmetic surgeon before your first meeting.
Never assume anything when it comes to your insurance policy. The only way to be certain is to get information directly from the source.
When you call the member services number on your insurance card, take detailed notes. Jot down the date, the representative's name, and a summary of your conversation. This log can be a lifesaver if any disagreements pop up later.
Here are the key questions to ask your insurance representative:
When it comes to insurance, the devil is often in the details. You can understand the big picture—the difference between cosmetic and reconstructive—but still have lingering questions about your specific situation. Let’s dive into some of the more common and sometimes tricky scenarios we see all the time.
Getting a handle on these finer points can be the difference between a smooth process and an unexpected, frustrating bill down the road.
Absolutely. This happens all the time with surgeries that serve a dual purpose, mixing functional needs with aesthetic goals. The classic example is a nose job, or rhinoplasty.
Imagine you need to fix a deviated septum to breathe properly, but you also want to refine the shape of your nose. In this case, insurance is likely to cover the medically necessary part—the septoplasty that improves your breathing. The cosmetic portion, however, will be your responsibility.
To manage this, your surgeon’s office will use what's called split billing. They'll create a detailed bill that separates the costs for the functional repair from the cosmetic changes. It's so important to talk this through with both your surgeon and your insurance company before surgery, so you know exactly what you’ll be expected to pay.
Whether your insurance will pick up the tab for your first visit with a plastic surgeon really boils down to one thing: why are you there?
A quick call to the surgeon’s office and your insurance provider ahead of time will clear up any confusion about their policies.
This one is a real shocker for patients. You did everything right, got your preauthorization, and then—bam—the final claim is denied. It’s confusing, but it happens.
A preauthorization is a green light, not a guarantee. It confirms that a procedure seems medically necessary based on the info submitted, but it doesn't promise the final bill will be paid no matter what.
So, why would a preauthorized claim get denied? It usually comes down to a few common culprits:
If you find yourself in this spot, don't panic. Your first call should be to your surgeon's billing office and your insurance company. Simple coding mistakes are often an easy fix. For bigger issues, you'll need to kick off the formal appeals process, and that preauthorization letter will be your single most important piece of evidence.
For smoothing wrinkles? No, never. But Botox has a whole other life as a legitimate medical treatment, and in those cases, insurance often steps in.
Insurance plans frequently cover Botox injections when they are proven to be the right medical solution for conditions like chronic migraines, severe underarm sweating (hyperhidrosis), and certain muscle spasm disorders. As long as your doctor provides solid documentation showing why it's medically necessary, these therapeutic uses are a different story entirely.
At Cape Cod Plastic Surgery, Dr. Fater and his experienced team can help you understand the nuances of your desired procedure, whether it's cosmetic or reconstructive. Schedule your consultation today to receive expert guidance on your aesthetic journey.

February 21, 2026
Discover how to prevent keloid scars after surgery with our definitive guide. Learn expert strategies for risk assessment, surgery, and post-op scar care.

February 20, 2026
What is Ultherapy treatment? Explore this non-surgical facelift, how it uses ultrasound to lift skin, and what results you can expect from the procedure.

February 19, 2026
Explore stunning cheek filler before and after results. See real patient photos, learn about filler types, and discover what's possible for your facial contour.