
March 3, 2026
Your Guide to the Cool Peel Laser Treatment
Discover the Cool Peel laser treatment. This guide explains how it delivers radiant skin with minimal downtime, what to expect, and who is an ideal candidate.
Jan 17, 2026

When you realize a chemical peel has gone wrong, what you do in the next 24 hours is absolutely critical. The right immediate steps can make a world of difference in your recovery, helping to calm angry skin and prevent a bad situation from getting much, much worse. Your goal right now is damage control—stabilizing the skin, not trying to fix the problem yourself.
If you think you're having a bad reaction, you need to go into crisis management mode for your skin. A calm, careful approach is key. The last thing you want to do is panic and start slathering on products that will only make the injury more severe.
Right now, the mission is simple: cool the skin down, reduce that fiery inflammation, and avoid putting anything on it that could trap heat or invite infection. Your skin's protective barrier has been seriously compromised, leaving it incredibly fragile.

While you're waiting to get professional help, a few simple actions can offer some relief and keep things from escalating. Just remember, these are temporary measures, not a replacement for a doctor's evaluation.
The biggest mistake people make is trying to treat a chemical peel burn with home remedies. When your skin is this compromised, less is always more. Gently cooling the area and getting an expert opinion fast are the most important things you can do.
Navigating the first few hours can feel overwhelming. Here’s a quick-reference table to guide your immediate actions and help you avoid common mistakes that could set back your healing.
Ultimately, what you don't do in these first few hours is just as important as what you do. The wrong move can easily lead to permanent scarring, infection, or hyperpigmentation.
Knowing the difference between a normal recovery and a real problem is key. It can be helpful to review expert advice on standard TCA peel post-care to see how your symptoms stack up against what's expected. Understanding a little about cellular regeneration—your body's incredible ability to repair itself—can also give you some perspective on the healing journey ahead.

After a peel, your skin is going to send you some pretty clear signals. The key is knowing how to translate them. Being able to tell the difference between a normal, productive healing process and the warning signs of a chemical peel gone wrong is the most important part of your recovery. It can mean the difference between a temporary inconvenience and a lasting complication.
Think of it this way: a good peel creates a controlled injury, like a mild sunburn that tells old, damaged skin it's time to go. A complication, on the other hand, is an uncontrolled injury—a chemical burn that's damaging deeper layers of your skin. Catching this early is everything. Having a basic grasp of what’s happening beneath the surface, including understanding skin inflammation and redness, helps you spot when things are going off track.
First, let’s establish a baseline for a typical recovery. If you're seeing these signs, your skin is most likely right on schedule.
These symptoms are all good signs. They tell you the treatment is doing exactly what it was designed to do and should get better with each passing day.
Now, let's talk about the serious stuff. These are the signs that are not part of a normal healing process. If you experience any of the following, don't wait and hope it improves—contact your provider immediately.
A burning sensation that gets worse over time, or doesn't calm down with a cool compress, is a huge red flag. Normal discomfort should be manageable and at its worst on the first day, not escalating after that. Intense, persistent pain is your body screaming that something is wrong.
Complications can show up right away or pop up weeks later. Medical studies consistently show that deeper peels come with much higher risks. Immediate issues include things like blistering and severe swelling, while delayed problems can be infections, scarring, or pigmentation changes. In fact, post-inflammatory hyperpigmentation can affect as many as 30-50% of patients with darker skin tones.
Here are the specific red flags you need to watch for:
Recognizing these signs early can completely change your outcome, stopping a minor issue from becoming permanent scarring or discoloration.
To figure out how to fix a chemical peel gone wrong, we first need to understand how it happens in the first place. A chemical peel isn't a simple facial; it's a controlled chemical wound designed to trigger a healing response. When any part of that process is mismanaged—even slightly—you can quickly go from controlled renewal to unintended damage.
Think of it like a carefully orchestrated chemistry experiment. The right ingredients, the right timing, and the right environment are all crucial. If you use the wrong acid for your skin type, leave it on a minute too long, or fail to protect the skin afterward, the experiment fails. It’s not about blame; it’s about knowing the variables so you can avoid a bad outcome next time.
One of the biggest culprits behind a bad peel is a simple mismatch between the acid used and the person's skin. Your skin has a unique history and biology, and a one-size-fits-all approach just doesn’t work here.
This is precisely why a detailed consultation with a board-certified specialist isn't just a suggestion—it's essential. They have the training to read your skin and choose a peel that will work with your biology, not against it.
The person holding the applicator is just as critical as the chemical in the bottle. With the boom in "medispas" and DIY at-home peels, we're unfortunately seeing more complications from sheer inexperience. More often than not, a chemical peel gone wrong can be traced back to someone who lacked the proper medical training.
An expert knows how to:
A chemical peel is a medical procedure, not just a facial. The person performing it must have a deep understanding of skin anatomy, wound healing, and chemistry to do it safely.
Finally, what you do after you walk out the door can make or break your results. Even a flawless peel can be sabotaged by poor aftercare. During that healing phase, your skin is fragile and incredibly vulnerable.
Here are the most common aftercare mistakes we see:
A great peel result is a partnership. It takes an expert provider to perform the treatment correctly and a dedicated patient who follows every post-care instruction to the letter. When one side of that partnership falters, the risk of a bad outcome skyrockets.
When you've done all you can with first aid at home and your skin still isn't recovering, it’s time to see a specialist. This isn't just a suggestion; it's the critical next step to stop lasting damage in its tracks and get your skin on the right path to healing. A board-certified plastic surgeon or dermatologist has an arsenal of treatments that simply aren't available over the counter, giving you a clear, professional roadmap back to healthy skin.
Think of it this way: a bad chemical peel is like an unexpected, damaging storm hitting the foundation of your house. Your specialist is the master builder who comes in to assess the situation, stabilize the structure, and carefully rebuild. The first step is always managing the immediate crisis, then we can shift focus to long-term repair.
First things first, we have to get the initial reaction under control. The immediate goal is to calm that angry inflammation, prevent infection from setting in, and create the best possible environment for your skin to start healing properly, without forming scars.
Depending on how severe the reaction is, your doctor might recommend:
Once the fire is out and your skin is stable, we can turn our attention to the lingering aftermath—things like scars or dark spots. This is where more advanced in-office procedures make a world of difference, but we only proceed once the skin is strong enough, usually weeks or months after the initial injury.
Scarring is easily one of the most dreaded complications from a botched chemical peel. It can turn what was meant to be a simple refresh into a serious reconstructive issue. While the risk of scarring from a superficial peel is less than 1%, deeper peels can carry a 5-10% risk, especially for certain skin types. You can discover more insights about peel complications from clinical reviews in dermatology journals.
Here are some of the go-to corrective treatments we use:
Dealing with the fallout from a bad chemical peel is undeniably stressful. But it’s so important to remember that there are powerful, effective medical solutions out there. With the right expert care, even significant complications can be managed and corrected, putting you on a clear path to restoring your skin's health and confidence.
When a chemical peel goes wrong, the recovery isn't a quick fix—it’s a journey. Think of it less like a sprint and more like a marathon. Understanding the distinct stages your skin will go through can make a huge difference in managing your expectations and easing the very natural anxiety that comes with a complicated recovery.
Patience is probably the most important tool you have right now. Your skin has an incredible ability to repair itself, but it works on its own schedule. Rushing the process at any point can cause setbacks, so respecting that natural pace is key to getting the best possible outcome.
This timeline gives you a roadmap for what to expect, from the immediate inflammatory response all the way through to long-term skin regeneration.
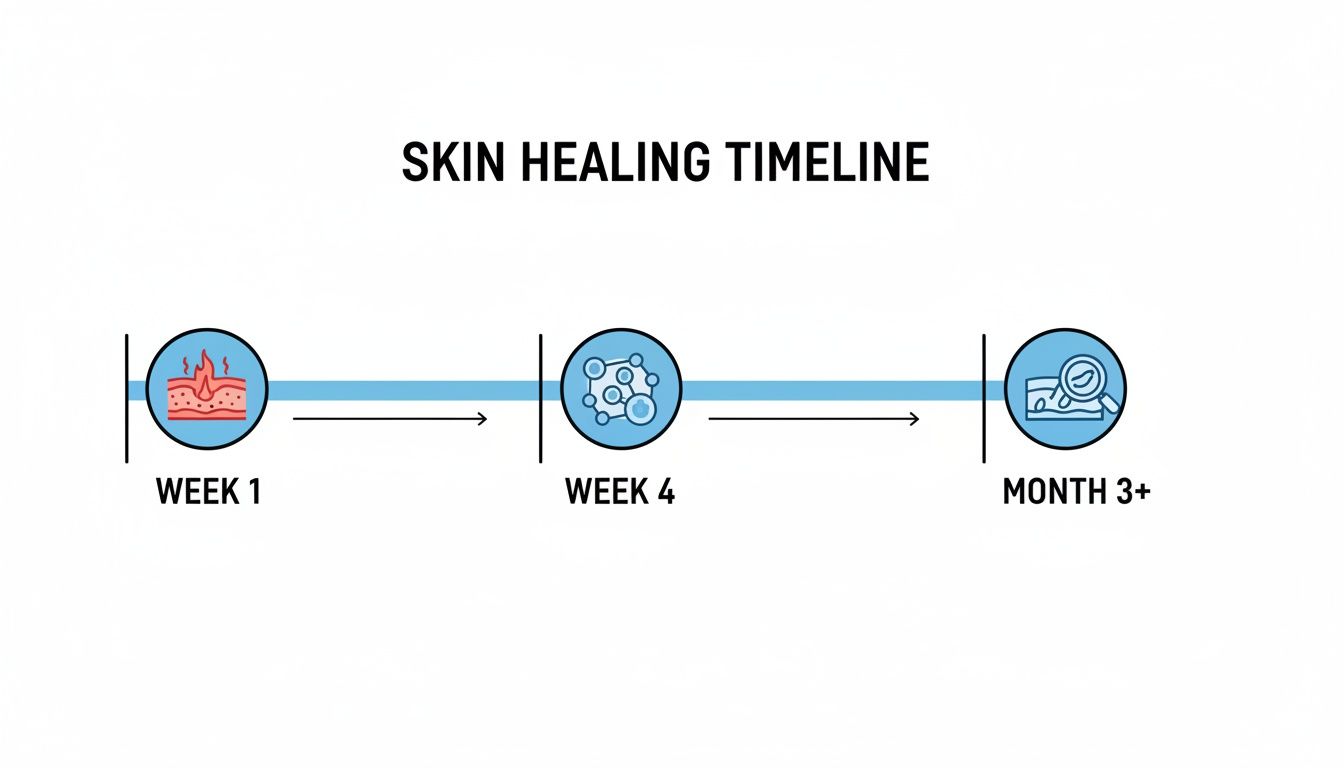
As you can see, healing is a progressive journey. It starts with intensive wound care in the first week and gradually shifts toward corrective treatments only after the skin is stable, which can be several months down the line.
The first 3-7 days are the most intense and, frankly, the most uncomfortable. Your skin is in full-blown crisis mode. Your only job is to create a calm, clean, and protected environment so it can start the delicate work of healing.
During this initial phase, your skin will likely be:
Your focus this week is simple: follow your doctor's wound care instructions to the letter. This isn't the time for improvisation. It means using only the prescribed cleanser, applying specific ointments, and avoiding the sun like the plague. Whatever you do, don't pick, scrub, or touch any blisters or peeling skin.
Once you get past that first week, the acute inflammation should start to calm down. Now the real rebuilding work begins, with new skin cells forming deep beneath the damaged surface.
This is what I often call the "ugly" phase of healing. Your skin might look patchy, discolored, and just plain uneven as it sheds in flakes or even sheets. It’s a messy but necessary part of the process. Trust it, and resist every urge to "help" it along by picking or peeling.
By the end of week four, most of the heavy peeling should be done. What’s left is brand new skin that is incredibly delicate, pink, and sensitive. The worst part is over, but this new skin is still extremely vulnerable. Sun protection becomes non-negotiable here, as even a few minutes of UV exposure can trigger significant, lasting hyperpigmentation.
From the second month on, the focus shifts from acute healing to long-term remodeling and correction. Your skin is much more stable, but now you’re likely dealing with the after-effects of the initial injury.
This is the stage where you might start to see:
At this point, your provider may determine it's finally safe to introduce gentle, corrective treatments. This could mean using medical-grade lightening agents for the PIH or starting specific therapies to improve texture. This remodeling phase is the longest, often lasting 6-12 months or more. It takes a long time for collagen to mature and for pigment to normalize, but with professional guidance and consistent care, real improvement is absolutely possible.
The single best way to recover from a chemical peel gone wrong? Do everything in your power to avoid one in the first place. While complications can happen even in the most experienced hands, your risk absolutely plummets when you choose a highly qualified provider. This isn’t the time to hunt for a bargain; it’s a medical procedure that demands a medical expert.
Think of it like this: you wouldn't hire a random handyman to fix your home's foundation. Your skin, the literal foundation of your appearance, deserves that same level of respect and expertise. Making an informed, safe choice is the most important thing you can do to protect your skin's health.
The first filter, and the most important one, is the provider's qualifications. Your search should start and end with professionals who have dedicated their careers to the science of skin. The absolute gold standard is a board-certified plastic surgeon or a board-certified dermatologist.
These specialists have gone through years of intense, supervised training focused on skin anatomy, wound healing, and complex aesthetic procedures. That kind of deep knowledge is exactly what's needed to correctly assess your skin and apply a peel safely and effectively.
A provider's credentials aren't just letters after their name. They represent years of dedicated training, proven knowledge, and a real commitment to patient safety. Board certification is the benchmark that proves they’ve met the highest standards in their field.
When you're looking into a potential provider, don't just take their word for it. You can, and should, verify their board certification online through official medical boards. This simple check gives you peace of mind and confirms you’re in truly expert hands. For a deeper dive into what these qualifications mean, check out our guide on how to choose a plastic surgeon.
The consultation before a peel is more than just a quick chat—it’s your chance to interview your potential provider. This is the time to dig in with detailed questions, get a feel for their experience, and see how they approach your specific skin concerns.
Here’s a checklist to bring to your meeting:
Your choice of provider is the most critical decision you'll make in this entire process. By making board certification a non-negotiable, asking sharp questions, and trusting your gut, you put yourself in the best possible position for beautiful, safe results.
When you're dealing with the fallout from a chemical peel gone wrong, it's natural to have a million questions running through your mind. It can feel overwhelming, so let's tackle some of the most common concerns head-on.
In most situations, the answer is a reassuring "yes." The real determining factors are the depth of the burn and how quickly you get in front of a medical professional. Superficial damage, when treated correctly and promptly, often heals without a trace.
Deeper burns are a different story and can sometimes leave behind permanent changes, like scarring or patches of discoloration. But even in these cases, all is not lost. Advanced treatments like laser therapy, microneedling, or prescription-strength creams can make a world of difference. The single most important thing you can do is get expert help immediately to map out a long-term recovery plan.
This is a tough one, because your first instinct is to fix the problem as fast as possible. But in this case, patience is truly a medical necessity. Your skin has to go through its initial, critical healing phase before it's strong enough for any kind of corrective work.
Jumping into another treatment—like a laser or even a gentler peel—too soon can easily make things much worse. This initial healing window can last anywhere from a few weeks to several months. Only a board-certified specialist can properly evaluate your skin's barrier function and tell you when it's stable enough to proceed. Rushing the process is a recipe for setbacks.
A common mistake we see is people trying to "fix" the damage with another procedure too quickly. Your skin needs to be fully healed and resilient before it can safely undergo any further intervention.
This is a really important question, and the answer depends entirely on why things went wrong the first time. If the complication came from something like an allergic reaction, poor aftercare, or an unqualified provider, you might be able to try a different, milder peel down the road—but only under strict medical supervision.
However, if it turns out your skin just isn't a good candidate for peels, or if you've developed significant scarring, this type of treatment might be off the table for good. A detailed consultation with an expert is the only way to figure out the safest path forward to meet your skincare goals without risking another chemical peel gone wrong.
At Cape Cod Plastic Surgery, Dr. Fater and our team prioritize patient safety above all else. If you're worried about a recent peel or want to explore rejuvenation options with a team you can trust, we're here to help. Schedule a consultation with a board-certified expert to get the right advice for your skin.

March 3, 2026
Discover the Cool Peel laser treatment. This guide explains how it delivers radiant skin with minimal downtime, what to expect, and who is an ideal candidate.

March 3, 2026
Essential Queries and Expert Guidance for Your Plastic Surgery Journey

March 3, 2026
Your Guide to Facial Rejuvenation on Cape Cod: Surgical and Non-Surgical Pathways