
February 9, 2026
How to Get Rid of Smile Lines for Smoother, Youthful Skin
Discover how to get rid of smile lines with our expert guide. We explore proven skincare, powerful injectables like fillers, and advanced treatment options.
Dec 6, 2025

While you'll likely be back to most of your gentle, day-to-day activities within 6 to 8 weeks, it's important to see that as just the first phase. Complete healing after breast reconstruction is a longer, more gradual journey, with the final results settling in over several months to a year.
Deciding to have breast reconstruction is a huge step, and knowing what to expect during recovery is key to feeling prepared and in control. It's helpful to think of your recovery not as a single event, but as a roadmap with different stages, each with its own set of milestones. Your personal path will be unique, shaped by your body, your overall health, and the specific surgical plan you and your surgeon decide on together.
The whole point is to feel prepared, not surprised. Understanding the timeline—from those first few days in the hospital to the moment you feel fully like yourself again—can make all the difference, reducing anxiety and empowering you to be an active partner in your own healing.
The biggest factor influencing your recovery timeline is the type of reconstruction you have. There are two main approaches, and they create very different healing experiences.
Grasping this fundamental difference is the first step in understanding what your personal breast reconstruction recovery will look like. It’s a major decision that directly affects everything from how long you're in the hospital to your final results.
It’s crucial to remember that "recovery" means different things at different stages. While healing from a mastectomy alone might take about four weeks, adding reconstruction extends that timeline. You can expect swelling and bruising to be part of the picture, and these usually take 6 to 8 weeks to go down. The deeper healing, where tissues fully settle and scars mature, is a much longer process—it can often take one to two years for scars to fade and soften to their final appearance.
For many women, especially when recovery is combined with other cancer treatments, the whole process can span several months. You can dive deeper into these timelines by reviewing expert insights on breast reconstruction.
"Your recovery is a marathon, not a sprint. The first few weeks are about rest and gentle healing, but the journey to feeling fully 'normal' again is a gradual process that unfolds over many months. Be patient and compassionate with yourself every step of the way."
We've put together this guide to give you a clear, straightforward overview. By breaking down the process, we hope to replace uncertainty with knowledge, helping you navigate your recovery with confidence.
To help you visualize your journey, here's a quick look at the key phases you can expect.
This table provides a quick reference to the typical phases of breast reconstruction recovery, helping you visualize your journey.
Remember, this table is a general guide. Your own timeline will be tailored to your specific procedure and how your body heals.
The first couple of months after your breast reconstruction are without a doubt the most intense part of your recovery, but it’s also when you’ll feel the most progress. Knowing what to expect week by week can make the whole process feel much less intimidating. Think of it as a roadmap for the first, most critical leg of your healing journey.
This timeline gives you a bird's-eye view of the major recovery phases, from those first few days in the hospital to the long-term settling of your final results.
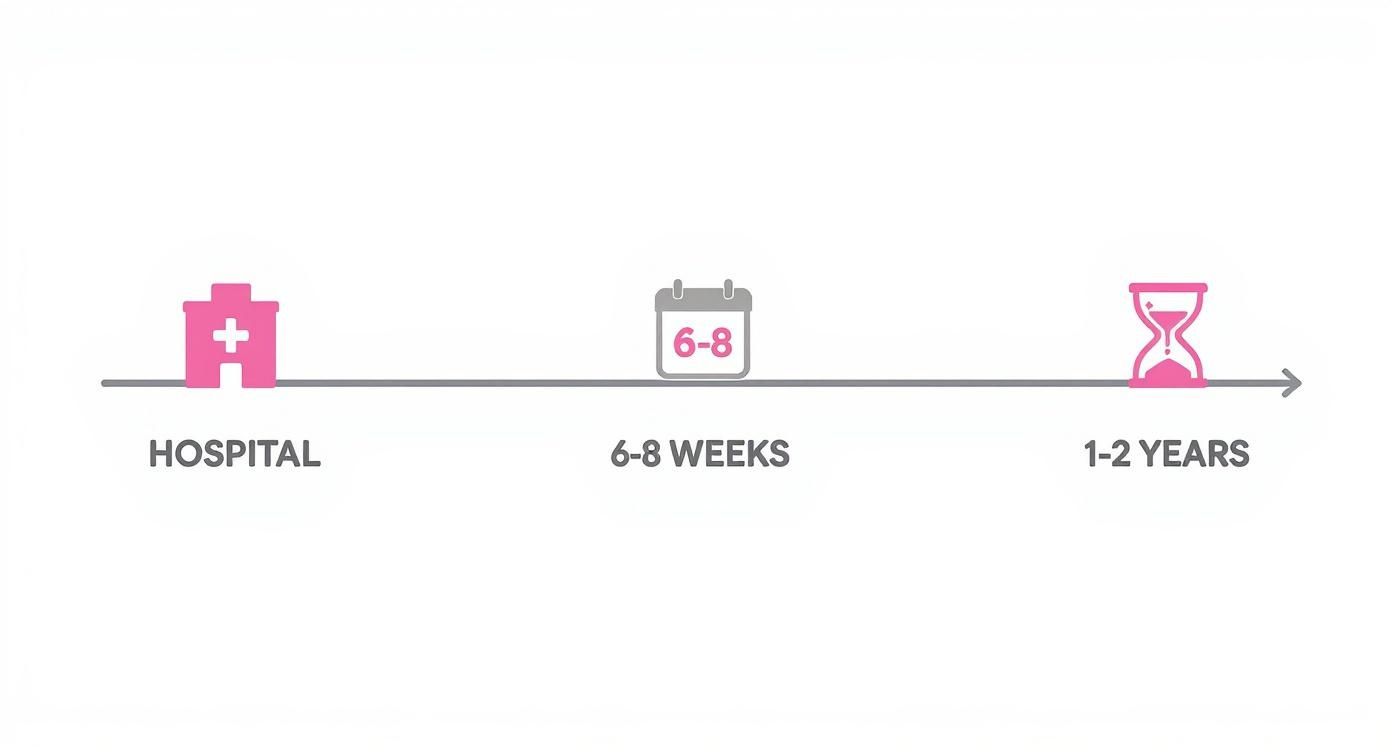
As you can see, the initial 6 to 8 weeks are all about active healing. But the full journey is a marathon, not a sprint. It often takes 1 to 2 years for scars to fully mature and for all the tissues to soften and settle into their final position.
These first two weeks are dedicated to one primary job: resting. Your hospital stay will typically be anywhere from 1 to 5 days, really depending on the type of reconstruction you had. Our focus during this time is simple: keeping you comfortable, watching your incisions closely, and making sure you know how to manage your surgical drains.
Once you’re home, your main responsibility is to take it easy. You’re going to feel tired, sore, and swollen—that’s completely normal. Your movement will be limited, and you’ll absolutely need some help with simple things like getting dressed or preparing meals. We do encourage you to take short, slow walks around your house to keep your circulation moving and help prevent blood clots.
A heads-up: Expect to feel a very real sense of tightness across your chest. This is a totally normal part of the process as your skin and muscles get used to their new shape, whether it’s from an implant or a tissue flap.
Your surgical drains will be your little sidekicks for a week or two. These thin tubes are essential for removing excess fluid from the surgery area, which prevents swelling and helps you heal properly. Before you go home, we’ll teach you exactly how to empty them and track the output for your surgeon.
This is when you’ll really start to feel like you’re getting back on your feet. The initial, sharp pain usually gives way to a more manageable ache and that feeling of tightness. Many of my patients find they can start tapering off the prescription pain medication around now and switch to over-the-counter options if needed.
A huge milestone often happens during this period: getting your drains removed! It’s a game-changer that makes everything from showering to just moving around so much easier.
This is a time of slowly re-engaging with your routine. The most important thing is to listen to your body and resist the urge to do too much, too soon.
In weeks five and six, you should notice your energy levels climbing. The swelling and bruising will have gone down significantly, giving you a much better preview of your new breast shape. Don’t be surprised if you feel some numbness—that’s common and can last for months. You might also feel some odd "zapping" or tingling sensations, which is actually a good sign that your nerves are starting to wake up.
Around this time, we’ll likely clear you for more activity. Lifting restrictions are often eased, and you can start incorporating longer walks or other low-impact exercises back into your routine.
Your focus during this time should be on:
By the end of the second month, you are officially on the home stretch of your initial recovery. The heavy lifting (figuratively and literally) of healing is mostly done. With your surgeon’s okay, you can typically get back to most of your normal activities, including more demanding exercise.
Even though you’ll feel worlds better, it’s important to remember your body is still healing on the inside. Your final results will continue to refine themselves over the coming months. It can take up to a full year for the last bit of swelling to disappear, and your scars will keep fading and softening for up to two years. Patience is still your best friend as your body finishes its incredible work.

Without a doubt, the single biggest factor that will shape your recovery journey is the type of reconstruction you and your surgeon decide on. It’s helpful to think of it like building a house. Are you using a high-quality prefabricated model, or are you building a custom home from the ground up? That analogy really gets to the core of the difference between implant-based and autologous flap reconstruction.
Each path comes with its own timeline and its own set of demands on your body. Understanding these key differences from the start is the best way to set realistic expectations and feel prepared for the road ahead.
Most women who choose reconstruction opt for an implant-based approach. This is usually a two-stage process. It starts by placing a tissue expander under the skin and muscle either during or after the mastectomy. Over the next several weeks, we gradually fill that expander, which gently creates a pocket for the permanent implant.
Because this method doesn’t require creating a second surgical site elsewhere on your body, the initial recovery is typically less demanding. It's like working with a pre-made kit—all the components are ready, so the work is focused in just one area.
This usually translates to:
The trade-off is that this path requires more appointments for the expander fills and at least one more surgery to replace the expander with the final implant. So, while the initial recovery is faster, the entire process can feel more drawn out over several months.
Autologous reconstruction, using techniques like a DIEP or TRAM flap, involves rebuilding the breast with your own tissue—most often from your abdomen. This is our "custom-built" approach. We meticulously transfer skin, fat, and blood vessels from the donor site to your chest, essentially sculpting a new breast mound.
This is a much more complex surgery, mainly because your body has to heal in two places at once: your chest and the donor site. That dual healing process naturally means the initial recovery time is longer.
Choosing an autologous flap reconstruction is a commitment to a more intensive initial recovery for a result that is entirely your own. The trade-off is a longer upfront healing period for a breast that can look and feel more natural over a lifetime.
If you go this route, you can generally expect:
While the upfront recovery is more involved, many women feel the long-term, natural-feeling results are well worth it. You can learn more about what goes into each procedure by exploring the various breast reconstruction options after mastectomy.
It’s not just about the first couple of months. The type of surgery also sets the course for your long-term healing. It's interesting to note that research shows the recovery journey is often longer and more complex than many women anticipate, no matter which method they choose.
One major study that followed patients found that many women, especially those with two-stage implant reconstructions, were still dealing with significant fatigue, pain, and upper body issues three months after their surgery. By contrast, patients who had autologous flap reconstructions often reported less pain and better physical well-being at that same three-month mark, despite having a tougher initial recovery.
What this tells us is that true functional healing—getting back to feeling like yourself—often takes much longer than the initial two-month window we tend to focus on.

Knowing what to expect during your breast reconstruction recovery is one thing, but having a few practical strategies up your sleeve can make all the difference. Beyond just getting your rest, there are simple, effective things you can do to manage discomfort and help your body heal.
The real secret is preparing before your surgery. By setting up your home and understanding the basics of post-op care ahead of time, you create a peaceful environment that lets you focus on one thing: getting better. From pain management to the clothes you wear, it’s the small details that add up to a much smoother experience.
Pain management will be one of your top priorities right after surgery. We’ll send you home with prescription medication for that initial period, but it's not the only tool you have. In my experience, a combination of approaches always works best.
How you position your body matters immensely. Many of our patients find that sleeping in a recliner or propped up with a wedge pillow is far more comfortable than lying flat. You can also tuck small, soft pillows under your arms for gentle support to take the pressure off your chest. It's also worth it to explore non-drug pain management options, like simple breathing exercises or meditation, to help calm your nervous system.
I always tell my patients to build a 'recovery nest.' Find a comfortable spot on the couch or in your bed and surround it with everything you might need: pillows, your phone charger, snacks, a big water bottle, and the remote. This prevents you from twisting or reaching for things, which is exactly what we want to avoid.
Taking good care of your incisions and surgical drains is absolutely critical. It’s your number one job in the early days of recovery and the best way to prevent complications. Our team will walk you through the specifics, and it’s so important to follow those instructions to the letter.
The surgical drains can be a bit of a nuisance, but they have an important job: removing fluid that would otherwise build up and cause swelling or infection. You'll need to empty them a few times a day and jot down the amount of fluid so we can track your progress. Just focus on keeping the skin around the drain sites clean and dry.
For your incisions, the goal is simple: keep them clean and protected. To learn more about the best ways to do this, check out our guide on how to care for surgical incisions. And always be on the lookout for early signs of infection, such as:
If you notice any of these, please call our office right away.
Don't underestimate the power of good nutrition in your recovery. Your body is working overtime to repair tissue, and it needs the right fuel to do its job well. Think of food as medicine during this time.
When you can't lift your arms very high, getting dressed can feel like a major task. The key is to forget about anything that pulls over your head for the first few weeks. Your wardrobe should be all about comfort and easy access.
Look for soft, loose tops that button or zip up the front. A zip-front hoodie or a comfortable cardigan with big pockets is a patient favorite—the pockets are a perfect, discreet place to tuck your surgical drains. For bottoms, think stretchy yoga pants or sweatpants with a soft waistband, especially if you had a flap procedure involving an abdominal incision. Planning this small detail makes a huge difference in your daily comfort and independence.
The physical healing after breast reconstruction is really only half the story. Your emotional journey is just as significant, and it’s a huge part of your overall recovery. It is completely normal to feel a whole mix of emotions during this time.
You might feel a wave of relief one moment and then frustration with your physical limits the next. You could feel gratitude alongside a sense of grief. These feelings can seem to contradict each other, but they are all a valid and expected part of the process. Your body has gone through a monumental change, and it makes sense that your mind needs time to catch up and process it all.
This isn't just about healing scars—it's about reconnecting with your body and settling into your "new normal."
You absolutely do not have to walk this path alone. In fact, one of the most powerful things you can have is a strong support system to see you through. This network can be anyone you trust: your family, close friends, or even other breast cancer survivors who just get it in a way no one else can.
Don’t ever be afraid to tell people exactly what you need. Sometimes that might be a practical thing, like a home-cooked meal. Other times, it might just be asking someone to sit with you in comfortable silence.
"Allowing yourself to be vulnerable and accept help is a sign of strength, not weakness. Your emotional wellbeing is just as important as your physical healing, and it deserves the same level of care and attention."
Many women also find that talking with a professional counselor makes a world of difference. A therapist can offer a safe, judgment-free space to unpack your feelings about body image, femininity, and your sense of self after surgery. They can give you coping strategies designed just for this experience. The link between our mental state and physical healing is profound, making it vital to understand the psychology of cosmetic surgery and its real-world effects.
It's common to feel a little disconnected from your body after reconstruction. It's going to look and feel different. You’ll likely have areas of numbness or other sensations that are totally new. This adjustment is a deeply personal experience, and there's no right or wrong way to feel about it.
This is where practicing self-compassion becomes so important. Try to give yourself grace and patience as you get to know your body again. Instead of zeroing in on perceived flaws, focus on what your incredible body has just endured and its amazing ability to heal. For many, reconstruction is a chance to redefine their relationship with their body, and resources that help you learn to love yourself can be a great help during this transition.
Here are a few gentle ways to help you reconnect:
Remember, your emotional recovery doesn’t have a deadline. Be kind to yourself, lean on your support system when you need to, and make sure to celebrate every small victory along the way.
Going through the recovery process for breast reconstruction naturally brings up a lot of questions. Knowing what to expect day-to-day can make a huge difference in how you feel and plan for the weeks ahead. Here are some of the most common things we talk about with our patients.
Getting back behind the wheel is a big milestone—it’s a return to independence. The green light for driving comes when two things are true: you're completely off any prescription pain medication, and you can comfortably and safely operate the car. This means turning the wheel sharply or checking over your shoulder without pain or hesitation.
For most people, this happens somewhere around 2 to 4 weeks after surgery. But remember, this is just a general guideline. You absolutely must get the official okay from your surgeon first, as your specific procedure and how you’re healing are the most important factors.
This is one of the most important rules to follow for a smooth recovery. You’ll need to avoid lifting anything heavier than a gallon of milk—which is about 8-10 pounds—for the first 4 to 6 weeks.
Sticking to this restriction is non-negotiable. It’s what protects your healing incisions and any internal muscle work. Pushing it too soon can lead to serious setbacks like bleeding, hernias, or shifting of your new breast mound or implant. We’ll give you very clear, personalized instructions on this.
Patience truly is a virtue during this process. You'll see your new breast shape right away, but what you see in the mirror on day one isn't the final look. It takes a good 6 to 12 months for all the post-surgical swelling to go down, for the tissues to soften, and for implants to fully settle into a more natural position—a process we often call the "drop and fluff."
And don't forget about your scars—they have their own journey. They will continue to fade and soften for up to two years after your surgery, becoming much less noticeable over time.
Think of that post-op surgical bra as your best friend for the first month or so. You should plan on wearing a supportive, comfortable, non-underwire bra 24/7 for at least the first 4 to 6 weeks, only taking it off to shower.
This round-the-clock support is critical. It does a few key jobs:
Our team will guide you on the exact type of bra to wear and for how long, all based on your specific surgery and needs.
At Cape Cod Plastic Surgery, Dr. Fater and our team are here for you at every single stage of your journey. If more questions come up or you’re ready to talk about what’s possible for you, please schedule a one-on-one consultation. To learn more about our philosophy of care, visit us at https://ccplasticsurgery.com.

February 9, 2026
Discover how to get rid of smile lines with our expert guide. We explore proven skincare, powerful injectables like fillers, and advanced treatment options.

February 9, 2026
Exploring Facial Cosmetic Surgery Options in Cape Cod
February 8, 2026
Explore the key differences in the breast reconstruction implants vs flap debate. This guide covers recovery, results, and risks to help you decide.