
February 9, 2026
How to Get Rid of Smile Lines for Smoother, Youthful Skin
Discover how to get rid of smile lines with our expert guide. We explore proven skincare, powerful injectables like fillers, and advanced treatment options.
Feb 8, 2026
When you're facing a mastectomy, one of the most significant decisions is how to move forward with reconstruction. The choice really boils down to two main avenues: breast reconstruction with implants vs. flap procedures.
At its core, the difference is straightforward. Implant-based reconstruction rebuilds the breast mound using saline or silicone devices. On the other hand, autologous flap reconstruction uses your own living tissue—usually from the abdomen or thighs—to create a result that feels incredibly natural. Deciding between them often comes down to what you value most: a quicker, less involved surgery (implants) or a permanent, more organic outcome that truly becomes part of you (flap).
Choosing your reconstruction method is an incredibly personal journey. It’s about more than just medical options; it’s about what fits your life, your body, and your vision for yourself after surgery. Our goal is to walk you through these two paths clearly and compassionately, so you can feel confident and empowered in your decision.

The two primary approaches couldn't be more different in technique, recovery, and what they feel like years down the road. Getting a real handle on these distinctions is the first step toward a productive conversation with your surgical team.
To give you a clearer picture of the trade-offs, here’s a simple breakdown of the key differences between breast reconstruction with implants and a flap procedure.
The most important goal is to find a solution that restores not just your shape, but your sense of wholeness. At Cape Cod Plastic Surgery, Dr. Marc Fater focuses on a patient-first approach, ensuring your choice aligns perfectly with your body, your health, and your life.
When you're facing breast reconstruction, the conversation almost always starts with two primary options: using implants or using your own body's tissue, often called a "flap" procedure. Think of these as two entirely different philosophies for rebuilding the breast. One relies on a carefully crafted medical device, while the other is a microsurgical marvel that relocates your own living tissue.
Your personal anatomy, your health history, and what you truly want out of your result will guide this decision. There's no single "best" choice, only the one that aligns with your body and your life. Let's break down what each path involves.
Implant-based reconstruction is the most common route taken in the United States. It's a method that rebuilds the breast shape using either silicone or saline implants, typically done in a two-stage process. This staged approach gives your body time to heal and adapt.
It usually starts with a tissue expander. This is an empty, balloon-like device placed under the chest muscle right after your mastectomy. Over the next few weeks and months, you'll come into the office for simple appointments where we gradually fill the expander with a sterile salt water solution. This process gently and slowly stretches the skin, creating the space needed for the final implant.
Once the skin has expanded enough, a second, much shorter surgery is scheduled to swap the expander for the permanent breast implant. You'll have choices to make here:
Implants also come in different shapes (round or teardrop) and with different surface textures (smooth or textured), all of which helps us customize the final look.
Autologous reconstruction, or flap surgery, is a completely different world. Instead of a device, we use a section of your own skin, fat, and blood vessels—a "flap"—to create a new, living breast. This tissue is most often taken from your lower abdomen, a bit like a "tummy tuck."
This is a delicate microsurgical procedure. We carefully disconnect the flap from its original location, move it to the chest, and then painstakingly reconnect its tiny blood vessels to a new blood supply there using a high-powered microscope. Because the new breast is made of your own living tissue, it will feel warm, soft, and natural. It will even change with you if you gain or lose weight.
Several types of flap procedures exist, named after the area the tissue is borrowed from:
Flap surgery is typically a one-and-done operation for creating the breast mound. The surgery itself is longer and the initial recovery is more involved, but the major advantage is that the result is permanent and doesn't require future surgeries to replace a device.
The choice is a significant one. For example, a major systematic review of outcomes found that while flap reconstruction can have more upfront surgical complications, it often results in greater long-term aesthetic satisfaction and psychological well-being. This really gets to the heart of the trade-off. You can explore the study's findings on flap and implant outcomes for a deeper look at the data.
When you're weighing your options for breast reconstruction, it's not just about the final result—it's about the entire journey. The path from your mastectomy through recovery looks very different for implant-based reconstruction compared to using your own tissue (a flap). Let's walk through what you can realistically expect, step by step.
The most immediate difference is in the operating room. An implant-based reconstruction starts with a much shorter, less complex surgery. The first stage, where we place tissue expanders, typically takes around 1-3 hours.
On the other hand, an autologous flap procedure is a more intricate microsurgery. It's a longer, more demanding operation for the surgical team, often lasting between 4 to 8 hours, sometimes even more. This time is spent meticulously moving the tissue and reconnecting tiny blood vessels to ensure the new breast has a living blood supply.
This initial surgical time directly impacts how long you'll be in the hospital. For implant reconstruction, many patients can go home the same day or after just one night. A flap reconstruction, being a more significant operation, requires a hospital stay of about 3-4 days. This allows us to closely monitor both your new breast and the area where we borrowed the tissue.
The first few weeks at home are where you'll really feel the difference. With implant reconstruction, the initial recovery is quicker. Most women are back to light, non-strenuous daily activities within 2-4 weeks.
Flap surgery recovery is more involved upfront. You're healing in two places at once—your chest and the donor site (often your abdomen). This means a longer initial healing period of 6-8 weeks is needed before you can get back to most of your normal routine. You can expect more significant pain management and mobility challenges during this time. You can learn more about managing this period by reading our detailed guide on https://www.ccplasticsurgery.com/blog/breast-reconstruction-recovery-time.
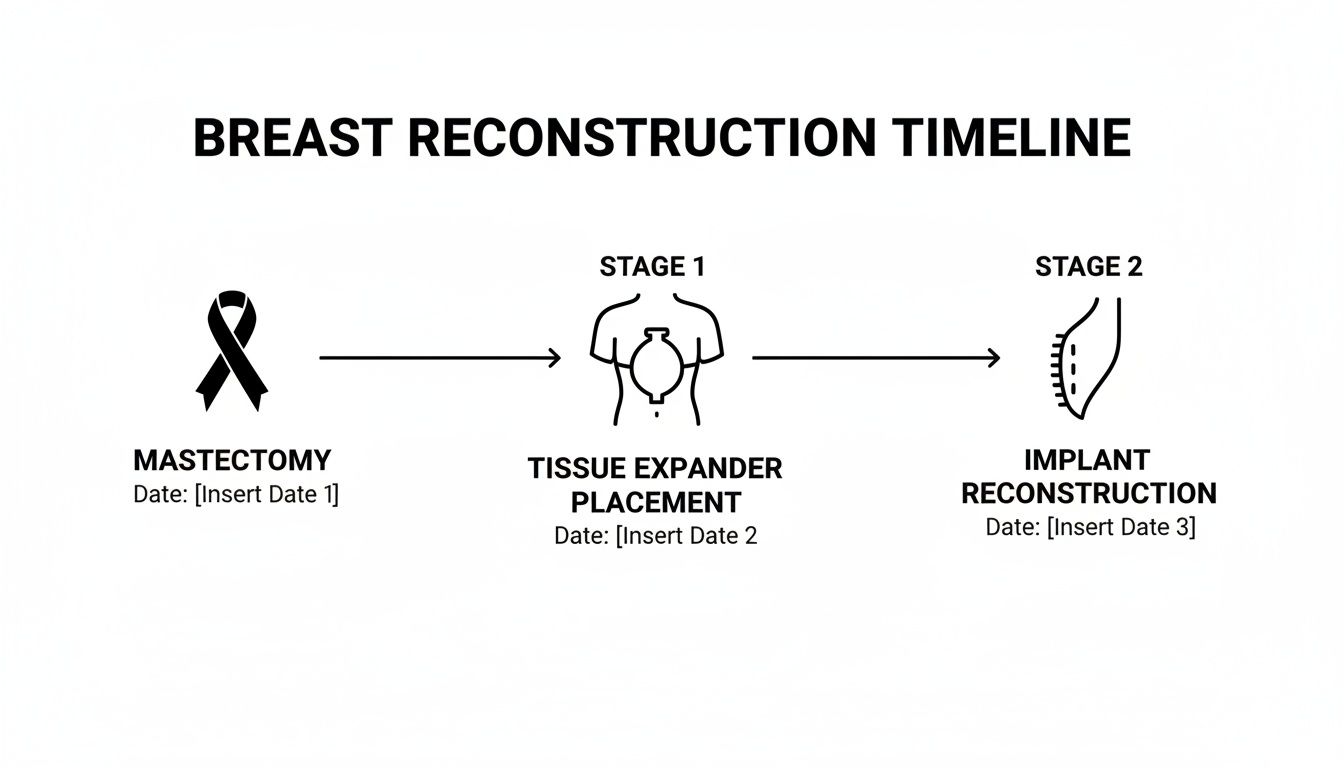
This timeline shows that while implant surgery starts with a quicker procedure, it's often a multi-stage process. Flap surgery, in contrast, is typically one major operation to create the breast mound.
To help visualize these key differences, here's a quick side-by-side comparison.
This table highlights the core trade-off: a faster initial recovery with implants versus a more intensive, but often one-time, procedure with flaps.
While flap surgery asks more of you upfront, it's often a "one-and-done" deal for creating the breast itself. Once that tissue is healed, it's a permanent and living part of you.
Implant reconstruction, while less intense at the start, often means more trips to the operating room down the line. The journey usually begins with a tissue expander, which is later swapped for a permanent implant in a second, shorter surgery. This multi-step path stretches out the total timeline.
The bottom line is this: Flap reconstruction has a tougher initial recovery, but implant reconstruction often involves a longer overall journey with multiple procedures over time.
This isn't just about convenience; it's about lifetime maintenance. Data shows a real difference in reoperation rates. Around 30% of breast implants might need to be removed within 10 years due to issues like severe scar tissue (capsular contracture) or device failure, with some studies showing reoperation rates as high as 45-50%. In contrast, modern DIEP flap procedures have success rates over 99% in the hands of an experienced microsurgeon, offering a durable solution without the risks associated with a foreign body.
Your return to physical activity will also follow a different script. After a flap procedure, you’ll have specific restrictions tied to the donor site. For example, if you had a DIEP flap from your abdomen, you'll need to avoid heavy lifting to protect those core muscles as they heal.
For implant patients, the focus is on the chest area. You'll need to limit upper body movements to give the implant pocket time to heal correctly. No matter which path you choose, a slow and steady return to exercise is key for your healing and strength. To help with this, resources like What Exercises Should You Do After Breast Cancer Surgery? can provide excellent guidance.
Ultimately, the choice comes down to what kind of journey you're prepared for. Do you prefer a less demanding surgery now, knowing you may need more procedures later? Or would you rather tackle a more involved operation and recovery for a permanent, single-stage solution? This is a deeply personal decision, and one we’ll help you make based on your health, lifestyle, and what matters most to you in the long run.
The initial surgery is just the beginning; you'll live with your reconstruction for a lifetime. When it comes to the long-term look and feel, implant-based and autologous flap procedures are truly worlds apart. One path gives you a defined, consistent shape, while the other creates a living part of you that will change and adapt right along with you.
The right choice really boils down to what you value most in your final result—predictable form or a natural, permanent feel. Getting to the heart of these differences is key to making a decision you’ll be confident in for years to come.
Perhaps the most significant difference is how each reconstruction feels and moves. An autologous flap reconstruction uses your own warm, living tissue—fat, skin, and sometimes muscle—to build a new breast. The result feels completely natural because, well, it is you.
Implants, on the other hand, are medical devices. While today’s implants are impressively sophisticated, they will always feel different from your own body tissue. They can feel firmer, sometimes a bit cool to the touch, and they won't have the same subtle drape or movement of a natural breast. For some women, though, the reliable shape and projection an implant provides are exactly what they're looking for, making this a worthwhile trade-off.
Key Insight: A flap reconstruction becomes a true part of you. It will gain or lose weight and age just as the rest of your body does. An implant remains static, which can eventually lead to asymmetry as your natural tissues change around it.
The idea of "permanence" is a huge factor in this decision. Flap surgery is undeniably a bigger operation upfront, but it's designed to be a one-and-done solution for creating the breast mound. Once the tissue has healed in its new home, it's there for life.
Implants, however, are not lifetime devices. They have a limited lifespan and come with the guarantee of future maintenance. Over the years, a few things can happen that will require another trip to the operating room.
Because of these potential issues, it's widely understood that implants often need to be replaced every 10 to 15 years. This means choosing implant reconstruction is also about planning for future surgeries down the road. To get a better handle on the devices themselves, you can learn more about the differences between silicone vs saline breast implants in our detailed guide.
What your new breast will look and feel like is, of course, paramount. Both techniques can produce beautiful outcomes, but the nature of those results is fundamentally different.
This comparison highlights the core trade-offs: implants offer a contained surgical footprint and predictable shape, while flaps provide a more integrated, living result at the cost of a donor site scar. That second scar is a real consideration for many patients, though surgeons are skilled at placing it where it can be hidden by clothing, and it typically fades well over time.
Ultimately, your personal priorities will guide your decision. If you want a permanent, natural-feeling breast and are prepared for a more complex initial surgery and recovery, a flap procedure could be your ideal match. If you prefer a simpler procedure with a faster recovery and are comfortable with the reality of future maintenance, a modern implant reconstruction can provide an excellent aesthetic result.
Deciding between implants and a flap procedure is a deeply personal conversation. There's no single "best" option—only what's best for you. The ideal candidate for one path often looks very different from the other, and it all comes down to your body, your health, and what you want for your future.
When you sit down with your surgeon, we'll look at a few key things together. We’ll start with your body type and see if you have enough tissue to "donate" for a flap. Just as important are your overall health and lifestyle, which tell us what kind of surgical journey you're best prepared for.
The most basic requirement for a flap procedure is simple: you need to have enough extra tissue in a donor area—usually the belly, thighs, or buttocks—to build a new breast. This naturally makes it a fantastic option for women who have sufficient body fat in those spots.
Beyond that, the best candidates for flap surgery often tell us they:
Flap reconstruction is also the go-to recommendation, and often a necessity, for women who have had radiation therapy.
Radiation changes the game. It makes the skin and chest tissue tighter, less flexible, and reduces its blood supply. Trying to place an implant in that environment is risky and can lead to problems like capsular contracture or poor healing. A flap, on the other hand, brings its own healthy, well-vascularized tissue to the chest, creating a much better foundation for a successful outcome.
Implant-based reconstruction is an excellent and reliable option for many women, especially those who aren't a good fit for flap surgery. The most common reason women choose this path is having a slimmer body type without enough extra tissue to spare.
You might be an ideal candidate for implants if:
While the surgery itself is less complex upfront, it’s crucial to be aware of the specific long-term risks. The most common issues we see are capsular contracture, where scar tissue around the implant becomes hard and tight, as well as the potential for infection or rupture.
It's an interesting trade-off. A Dutch study revealed that while flap reconstruction had a higher risk of major complications right after surgery (27% vs. 12% for implants), the women who chose the flap procedure reported being much happier with their results in the long run. This really speaks to the balance between upfront surgical intensity and long-term quality of life. You can dig deeper into these findings on flap reconstruction outcomes to learn more.
Ultimately, the choice is one we make together. A thorough consultation here at Cape Cod Plastic Surgery will help us weigh your unique anatomy, health history, and personal goals to find the path that offers you the safest journey and the most satisfying result.
Deciding between implant-based and flap reconstruction is a deeply personal journey. There really is no single "best" answer that fits everyone. The right path forward is the one that truly aligns with your body, your lifestyle, and what you envision for your own healing and sense of wholeness. It’s a choice that weaves together medical facts with your individual priorities.
To move forward with confidence, the most important step is having a frank, open conversation with your surgeon. Taking some time to reflect on your own priorities beforehand will make that discussion incredibly productive and ensure the plan we create together is one you feel great about.
Preparing a little for your consultation can help you clarify what matters most to you. Think of these questions as a starting point to guide both your internal reflection and your conversation with the surgical team:
The most important outcome is a reconstruction that restores not just your physical form, but your sense of self. The "right" choice is the one that brings you peace of mind for years to come.
Here at Cape Cod Plastic Surgery, we view this decision as a true partnership. Dr. Marc Fater brings over 30 years of board-certified experience to every consultation, so you can be sure you’re receiving guidance grounded in deep expertise and a total commitment to your safety. He will help you weigh every aspect of the breast reconstruction implants vs flap debate, all within the context of your unique situation.
Our team can also help you navigate the practical side of things, like understanding how insurance can assist with the costs. You can learn more in our guide on insurance coverage for plastic surgery.
Our entire practice is built on personalized care. From your first conversation to your final follow-up, it all happens right here in our on-site, AAAASF-accredited surgical suite. Together, we’ll create a plan that honors your body and helps you move forward with confidence and clarity.
When you're thinking about breast reconstruction, a lot of very real, practical questions come up. It's completely normal. Getting answers to these common concerns is one of the most important steps in feeling sure about your path forward, whether it's with implants or a flap procedure.
Let's walk through some of the questions we hear most often from our patients here on the Cape.
This is a big one, and it's smart to have realistic expectations from the start. During a mastectomy, the nerves that provide sensation to the breast skin are cut. This means that with either an implant or a standard flap reconstruction, feeling in the breast area will be significantly reduced, if not gone entirely.
However, flap reconstruction does offer a unique possibility here. Some advanced microsurgical techniques allow us to actually reconnect sensory nerves during the procedure. It's delicate work, and it's not a guarantee, but it opens the door for some feeling to return over time—a possibility that just doesn't exist with an implant.
We can never restore sensation completely, but for many women, regaining even a little bit of feeling helps them feel more like themselves again. It can make a world of difference.
If you've had or will need radiation therapy, it's a game-changer for your reconstruction options. Radiation makes the skin and underlying tissue tighter, less elastic, and reduces its blood supply. This creates a really tough environment for a breast implant to succeed.
Trying to place an implant under radiated tissue comes with a much higher risk of problems, including:
Because of these risks, using your own tissue in a flap reconstruction is almost always the safer, more reliable choice after radiation. A flap brings in its own healthy, robust blood supply, creating a soft, natural result that is built to last in a way an implant just can't in radiated tissue.
Yes, it absolutely should. Breast reconstruction after a mastectomy is not considered a cosmetic procedure; it's a fundamental part of your cancer treatment and recovery.
A federal law called the Women's Health and Cancer Rights Act of 1998 (WHCRA) makes this clear. This law requires most group health plans that cover mastectomies to also cover all stages of breast reconstruction. That means the surgery to rebuild the breast, any work needed on the other breast to create symmetry, and prostheses are all included. We always help our patients confirm the specifics with their insurance provider, but coverage is the standard.
At Cape Cod Plastic Surgery, Dr. Fater will sit down with you to go over all these questions and more, offering guidance that’s specific to your health and your goals. Schedule your personal consultation today so we can start creating the right reconstruction plan for you.

February 9, 2026
Discover how to get rid of smile lines with our expert guide. We explore proven skincare, powerful injectables like fillers, and advanced treatment options.

February 9, 2026
Exploring Facial Cosmetic Surgery Options in Cape Cod
February 8, 2026
Explore the key differences in the breast reconstruction implants vs flap debate. This guide covers recovery, results, and risks to help you decide.