
February 24, 2026
7 Revealing Buccal Fat Removal Before And After Examples (2026)
Explore our curated gallery of buccal fat removal before and after results. See real patient outcomes, understand candidacy, and learn what to expect.
Jan 10, 2026

A successful recovery from plastic surgery is a journey that truly begins weeks before you ever step into the operating room. The outcome you're hoping for is built on a foundation of proactive preparation. Getting your body ready, setting up your home, and lining up a solid support system are just as important as the procedure itself. Honestly, taking these steps seriously can make a world of difference in your healing and peace of mind.
A comfortable, low-stress recovery doesn’t just happen—it’s the direct result of thoughtful planning. Everything you do beforehand directly influences how well, and how quickly, you heal in those crucial first days and weeks. Think of this pre-op phase as your head start on the healing process.
This isn't just about blocking out your calendar. It’s a holistic approach that covers your physical health, your mental readiness, and your living space. By getting these pieces in place now, you're empowering yourself to navigate recovery with confidence, especially when you're feeling most vulnerable.
Your body is about to do some serious work, and giving it the right fuel is non-negotiable. Healing demands a ton of energy and specific nutrients, especially protein, which is the absolute building block for tissue repair. In the weeks leading up to your surgery, make a conscious effort to eat lean proteins like chicken, fish, beans, and tofu with every meal.
Hydration is just as critical. Staying well-hydrated keeps your blood flowing efficiently, which is how oxygen and vital nutrients get to the surgical site to work their magic. Aim to sip water consistently throughout the day. You’ll also want to cut back on things like excessive caffeine that can dehydrate you.
We will give you a very specific list of medications and supplements to stop taking before your surgery. This is a big deal. The list almost always includes:
Your pre-operative instructions aren't just suggestions; they are a critical part of your safety protocol. Following them to the letter is one of the most important things you can do to ensure a great outcome.
Your home should be your haven, set up for maximum rest and minimal effort. You'll be conserving all your energy for healing those first few days, so getting your space ready beforehand is a game-changer. Pick one spot to be your main recovery area—your bed or a comfy recliner—and bring everything you’ll need within easy reach.
I always tell my patients to create a "recovery station" on a nightstand or small table. Stock it with essentials like:
Prep the rest of your home, too. Clear the walkways to the bathroom and kitchen so you don't trip over anything. If you’re having a procedure like a tummy tuck that limits your mobility, move frequently used items from high cupboards to the counter so you aren't tempted to stretch or strain. For a more detailed list, our guide on how to prepare for surgery has a fantastic checklist to follow.
You'll also be living in compression garments for a bit to help control swelling and support your results. It's worth looking into your options ahead of time. Understanding what makes for good postpartum shapewear for recovery, for example, can be incredibly helpful as you plan for your post-op needs.
Let's be clear: you won't be able to do this alone, especially in the first 24 to 72 hours. You absolutely must arrange for a trusted friend or family member to drive you home and, ideally, stay with you for at least that first night. This person is your lifeline—they’ll help with medications, bring you food, and assist with simple things you won't be able to manage.
Have a frank conversation with your designated caregiver before the big day. Let them know what your limitations will be and what they can realistically expect. Give them our contact information and a copy of your post-op instructions. The more prepared they are, the better they can help you navigate those first few critical days.
That first week after your procedure is intense, and it’s where all your careful preparation really comes into play. Think of this period as your dedicated healing phase—your only job is to rest, manage your comfort, and let your body do its work. It’s crucial to follow your post-op instructions to the letter and, just as importantly, listen to what your body is telling you.
Right after surgery, you’re going to feel tired, groggy, and sore. That’s perfectly normal. The anesthesia needs time to wear off, and your focus will be on getting settled at home with your support person. Now is not the time to be tough; let your helper do everything, from grabbing you a glass of water to keeping your medication schedule on track.
The first two days are all about rest, period. You’ll likely spend most of this time sleeping or resting in a propped-up position, which is key to keeping swelling down. Don’t be surprised by what you see in the mirror—swelling and bruising are completely expected and tend to hit their peak during these initial days.
Your top priority here is pain management. We can't stress this enough: you must stay ahead of the pain by taking your prescribed medication on a strict schedule. If you wait until the pain gets bad, you’ll have a much harder time getting comfortable again. I tell all my patients to set alarms on their phones, even overnight, so they don’t miss a dose.
For a more detailed breakdown, we’ve put together a guide with more strategies on effective pain management after surgery to help you through.
Around day three, you’ll probably start to feel a little more like yourself again. You'll still be sore and moving slowly, but the fog will begin to lift. For many, swelling can hit its peak around this time before it finally starts to go down. It's also common to feel a bit impatient or even down—the emotional side of recovery is very real.
This is the perfect time to start taking very short, gentle walks around the house every hour or so while you're awake. This isn't exercise; it's about boosting your circulation to help prevent complications like blood clots. A slow stroll from the couch to the kitchen and back is all you need.
Your only goals for this first week are to rest, hydrate, eat nourishing foods, and manage your pain. Pushing yourself too soon is the quickest way to set back your recovery.
A smooth first week is almost always the result of solid planning before surgery day.
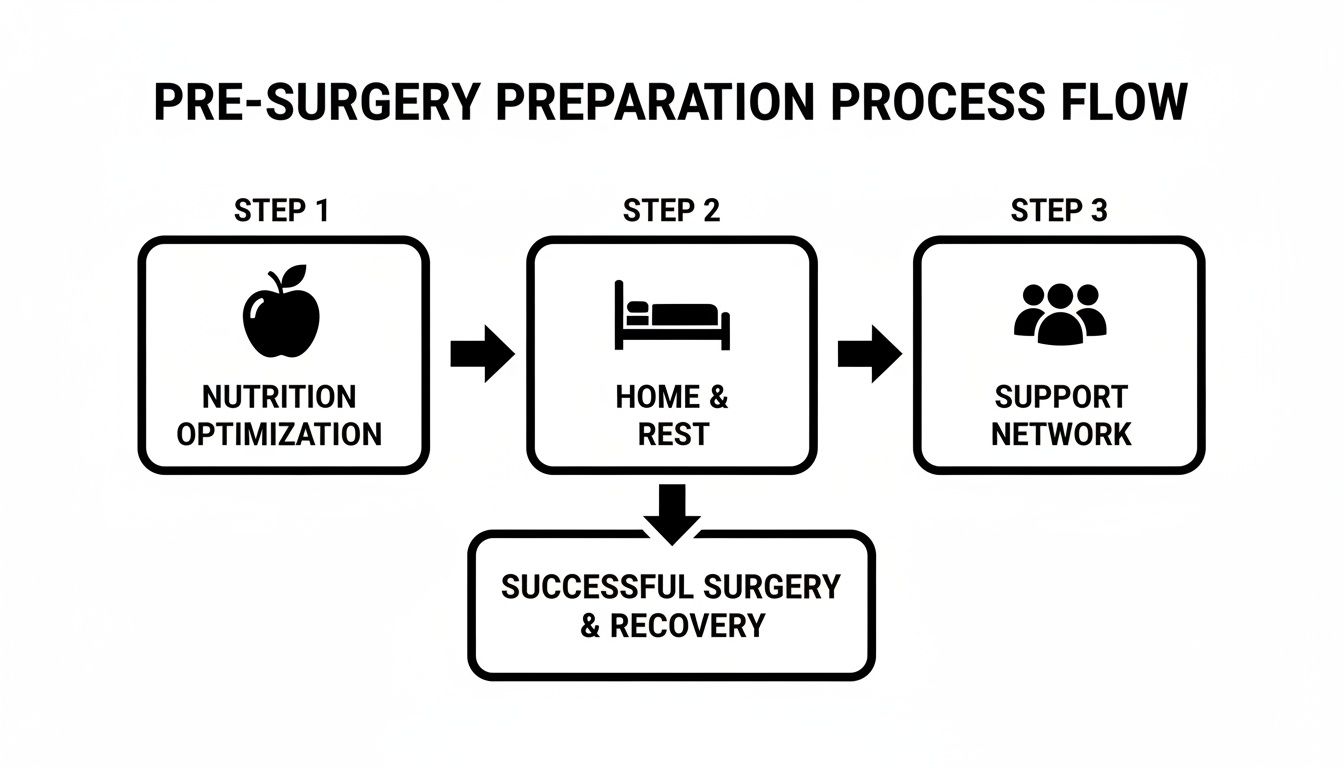
This visual really breaks down the pillars of a successful recovery: getting your nutrition right, setting up a comfortable and restful space at home, and, most importantly, having a reliable support person lined up. Getting these things sorted out beforehand makes all the difference.
To help you visualize the week, here's a quick cheat sheet for what to prioritize day by day.
This table is just a general guide, but it gives you a good idea of the rhythm of that initial healing period.
As you round out the first week, you should feel a real shift. Your pain should be much more manageable, and you might even be ready to switch from prescription medications to something over-the-counter like Tylenol. Just make sure you get the green light from us first. You’ll feel more confident moving around and handling your own basic needs.
Now's the time to keep a close eye on your incisions and any drains you might have. Follow the care instructions we gave you precisely—this usually involves simple cleaning and watching for any red flags.
You're in good company on this journey. In 2023 alone, surgeons in the United States performed 6.2 million reconstructive procedures, which is over 24% of all aesthetic procedures done globally. That vast experience means that we have incredibly refined recovery protocols designed to get you through this process safely and with the best possible outcome.
Your first follow-up appointment is usually scheduled for about a week after your surgery. We'll check on your healing, take out any stitches if needed, and make sure all your questions are answered. Getting through this first week is a huge milestone—be proud of how far you've come.
Once you’re past that first week, you’ll find the intensity of your initial recovery starts to soften. This next phase, from week two all the way to week six, is really about gradual progress and slowly getting back into a more familiar rhythm. You'll start feeling more like yourself, but this is a time that still demands a lot of patience and listening carefully to what your body is telling you.
This is when you can finally see the light at the end of the tunnel. Swelling and some bruising will still be hanging around, but you'll notice them going down week by week. Watching your results slowly reveal themselves is incredibly exciting, but you have to manage your expectations as your body is still doing some serious work behind the scenes.

Your first big follow-up appointment usually falls right at the start of this period, and it's a huge step forward. At this visit, we'll take a close look at how you're healing, check your incisions, and get rid of any remaining stitches or surgical drains.
Getting those drains out, if you had them, brings an immediate feeling of relief and freedom. It's also perfectly normal for some fluid to keep accumulating, so don't be alarmed if you still see some swelling. It’s all part of the process.
To get the most out of this appointment, come prepared. Jot down any questions you have—nothing is too small or silly to ask. You might want to ask about:
Remember, this is a partnership. Your own observations are incredibly valuable, so please be open and honest about how you're feeling.
Movement is absolutely essential for a smooth recovery, but you have to ease back into it. During weeks two through six, you’ll get the green light to venture beyond short walks around the house. Think of gentle, sustained walking as your best friend right now.
Start with short, 10-15 minute walks on flat ground. As you feel stronger, you can gradually go a little longer or further. Walking is fantastic for promoting healthy blood flow, which speeds up healing, brings down swelling, and significantly lowers the risk of complications.
Important Takeaway: The number one rule is to listen to your body. If you feel any sharp pain, pulling sensations, or just plain exhaustion, that's your cue to stop and rest. Pushing through pain will only set your recovery back.
While walking is great, many other activities are still off-limits. You absolutely must continue to avoid:
Sticking to these rules is non-negotiable. It's how we protect your incisions and ensure you get the beautiful results you’re working toward.
Swelling is by far the most persistent guest during this stage. The worst of it is usually over after the first couple of weeks, but some residual puffiness can stick around for months, especially after procedures like tummy tucks or liposuction.
As you move through this period, some specialized massage techniques can be a huge help in reducing that lingering swelling. You can find excellent guidance on lymphatic drainage massage, which we often recommend to help move stagnant fluid and refine your new contours. Just be sure to get our approval before you start any kind of massage therapy.
Emotionally, this can be a bit of a rollercoaster. It’s a thrill to see your new shape emerge, but it can also be frustrating when it feels like the final results are taking forever. You'll likely have days where you feel more swollen than the day before—that's completely normal and often has to do with your activity level or even how much salt you ate.
Try to practice patience and focus on the small, daily improvements. Your body has been through a major event and it needs time to heal and settle. Taking a quick photo once a week can be a fantastic way to track your progress and see just how far you've come, especially when the day-to-day changes feel tiny. This is a marathon, not a sprint.
The first few weeks after surgery are all about rest and initial healing, but what happens after that? Think of the first six weeks as laying the foundation. Everything that follows is about protecting that investment for the long haul. The habits you start building now will directly influence how great your results look years down the road.
Your surgery isn't a temporary fix; it's your new starting point. Maintaining it means committing to a lifestyle that supports both your physical results and your overall well-being. This is where you truly take ownership of your new look and make it last a lifetime.

Scars are an unavoidable part of most procedures, but how they ultimately look is very much in your hands. At first, your scar will be red and maybe a little raised—that’s completely normal. Over the next six to twelve months, it will slowly mature, becoming softer, flatter, and lighter in color.
Your two best friends during this phase are sunscreen and silicone.
Sun Protection is Non-Negotiable: A new scar is incredibly sensitive to UV rays. Sun exposure can cause it to darken permanently (hyperpigmentation), making it far more noticeable. For at least the first year, you absolutely must apply a broad-spectrum SPF 30+ sunscreen anytime the scar might see the sun.
Silicone Is the Gold Standard: Once your incision has fully closed and we give you the green light (usually around 3-4 weeks post-op), it's time to start using silicone. Whether you choose sheets or gels, they are clinically proven to improve a scar's appearance by hydrating the tissue and regulating collagen. The key is consistent, daily use.
Your scar's final appearance is a marathon, not a sprint. Be patient and stick with your scar care routine for at least a year. The long-term payoff is a minimal, well-healed line that tells a subtle story of your transformation.
Once you’re cleared of major restrictions around the six-week mark, you can start easing back into a full exercise routine. A common mistake we see is people jumping back in too fast, which can seriously compromise results, especially after procedures like a tummy tuck or breast augmentation.
The goal here is to rebuild your strength slowly and deliberately, without putting any unnecessary strain on your healing body.
Weeks 6-12: A Phased Approach
Remember, your core will likely be much weaker, particularly after an abdominoplasty where we’ve repaired the muscles. Avoid any intense, direct ab work like crunches or planks until your surgeon gives you specific approval—which could be three months or more post-op.
The final—and arguably most important—piece of the puzzle is your day-to-day lifestyle. Your beautiful new contours can be affected by major weight fluctuations, poor diet, and your general health. To protect your investment, you need to adopt habits that support your new shape for good.
A stable weight is crucial. A balanced diet centered on whole foods will help you maintain your results and prevent the skin from stretching. Staying well-hydrated is also fantastic for your skin’s elasticity and health.
Try to think of healthy eating and regular exercise not as chores, but as the essential maintenance that keeps your surgical results looking their absolute best. By making these practices a part of your life, you ensure that the confidence and happiness you feel today will be with you for years to come.
Think of your recovery as a partnership. We're here to guide you, but you're in the driver's seat when it comes to monitoring your own healing. It's crucial to understand the difference between what’s normal and what’s a red flag.
Most of what you’ll feel—some swelling, bruising, and manageable discomfort—is just your body's natural way of healing. But staying alert helps you spot potential issues early, which is the key to a smooth and successful outcome. You're the most important member of your care team.
Infection is a common concern after any surgery, but the good news is that it’s highly preventable when you follow your aftercare plan. The trick is catching the signs before they escalate.
While some redness directly along an incision is expected, an infection looks and feels different. You should be watching for symptoms that get worse over a day or two, not better.
A hematoma is a pocket of blood that collects under the skin, and a seroma is a similar collection of clear fluid. Some fluid is a normal part of the healing process, but a large, sudden buildup needs our attention.
A hematoma often appears as a sudden, firm, and painful swelling in one specific spot. The pain is usually sharp and feels out of proportion to your overall discomfort. A seroma might feel more like a small water balloon under your skin. If you notice any dramatic, localized swelling, it's time to pick up the phone.
Your intuition is one of your most valuable recovery tools. If something just doesn't feel right, please don't hesitate to contact us. It's always better to call and be told everything is normal than to wait and let a small issue become a bigger one.
Deep vein thrombosis (DVT), or a blood clot in the leg, is a serious but less common risk. This is exactly why we encourage you to get up and walk around gently as soon as you’re able. To learn more about proactive steps, check out our guide on preventing blood clots after surgery.
The warning signs of a DVT almost always appear in just one leg. Look out for these symptoms in your calf or thigh:
The field of plastic surgery has come a long way. The number of procedures performed more than doubled between 1999 and 2018, and this growth has led to incredible advancements in safety protocols and patient care. Today’s recovery process is safer and more predictable than ever before.
We are with you every step of this journey. Keep our number handy, and remember these key warning signs. Knowing when to call will give you the peace of mind to focus on what matters most: resting and healing.
As you move through the healing process, you’re bound to have questions pop up. It’s completely normal. To help you feel more prepared, we’ve put together answers to some of the most common questions we hear from our patients every day.
Let's be direct: the first two to four days are usually the toughest. That's when you'll experience the most significant discomfort. The single best piece of advice I can give is to stay ahead of the pain. Take your prescribed medication on the dot, as scheduled—don't wait for the pain to ramp up before you take it.
After those first few days, you'll notice a real shift. Most patients find they can comfortably switch to over-the-counter options like Tylenol to manage the lingering soreness. And don't forget the simple things; a well-placed cold compress can work wonders for localized swelling and pain.
This is a big milestone for everyone, but the timing is completely tied to the specifics of your surgery. For many procedures, you might get the okay to shower within 48 to 72 hours.
However, if you have surgical drains or special dressings, you'll have to wait a bit longer. The absolute priority is keeping your incisions dry to prevent infection. Your team here at Cape Cod Plastic Surgery will give you crystal-clear instructions tailored just for you. Following their guidance is non-negotiable for a safe recovery.
This is the part where patience truly becomes your best friend. You'll see a change right away, of course, but swelling and bruising are going to obscure the final look for a while.
By the six-week mark, most of the major swelling has gone down, and you’ll have a really good preview of your new shape. But the last little bit of refinement—that subtle settling of tissues—can take anywhere from six months to a full year, especially for procedures like a tummy tuck or rhinoplasty. It’s a marathon, not a sprint.
Your healing journey is yours alone. It’s so easy to compare your progress to photos online, but it’s the worst thing you can do. Focus on your body, celebrate your own milestones, and trust the process.
Great question. Your scar care strategy really has two distinct phases.
For the first few weeks, your only job is to follow your incision care instructions to the letter. Keeping the area clean and protected is the foundation for everything that comes next.
Once you get the green light from your surgeon at a follow-up appointment, you’ll shift into long-term scar management. This is where you can make a huge difference:
We'll map out a specific scar care plan for you based on your surgery and skin type. Following it diligently is the surest way to help your scars heal beautifully and discreetly.
At Cape Cod Plastic Surgery, we know that feeling prepared is the key to a smoother recovery. If you have more questions about what to expect after your plastic surgery procedure, we encourage you to schedule a personalized consultation with Dr. Fater. We're here to help you begin your journey with confidence.

February 24, 2026
Explore our curated gallery of buccal fat removal before and after results. See real patient outcomes, understand candidacy, and learn what to expect.

February 23, 2026
Discover how to reduce frown lines with expert-backed tips on skincare, lifestyle changes, and professional treatments that deliver real, lasting results.

February 22, 2026
Learn how to minimize bruising after surgery with our expert guide. We share preoperative and postoperative tips for a faster, smoother recovery.